Nutritional and Functional Medicine Approach for Ataxia
Ataxia is defined as an inability to coordinate muscle movements, resulting in lack of coordination or unsteadiness usually related to a disturbance in the cerebellum, a part of the brain that regulates coordination and equilibrium. The condition may result from various diseases of the cerebellum, or from abnormalities affecting other areas of the brain or central nervous system, ataxia often stems from underlying nutritional deficiencies, mitochondrial dysfunction, or toxin exposure. Research has shown that deficiencies in vitamins like thiamine (B1), B12, and essential fatty acids impair nerve function, while mitochondrial dysfunction reduces energy available for motor control. A functional medicine approach, focusing on addressing root causes like nutrient imbalances and gut health, offers a holistic solution. In this blog, we explore how targeted nutrition and functional medicine strategies help improve symptoms and enhance the quality of life for those with ataxia.
Understanding Ataxia
Ataxia is a neurological disorder characterized by uncoordinated movements, impaired balance, and difficulty with motor tasks like walking or speaking. While ataxia is often genetic, it often arises from other causes like nutritional deficiencies (e.g., thiamine, vitamin B12), mitochondrial dysfunction, or toxin exposure (heavy metals, alcohol). Neurological factors, such as damage to the cerebellum, disrupt the body’s control over movement. Additionally, metabolic issues like impaired mitochondrial function limit energy production in the brain, worsening ataxia symptoms. Addressing these root causes is crucial for effective management
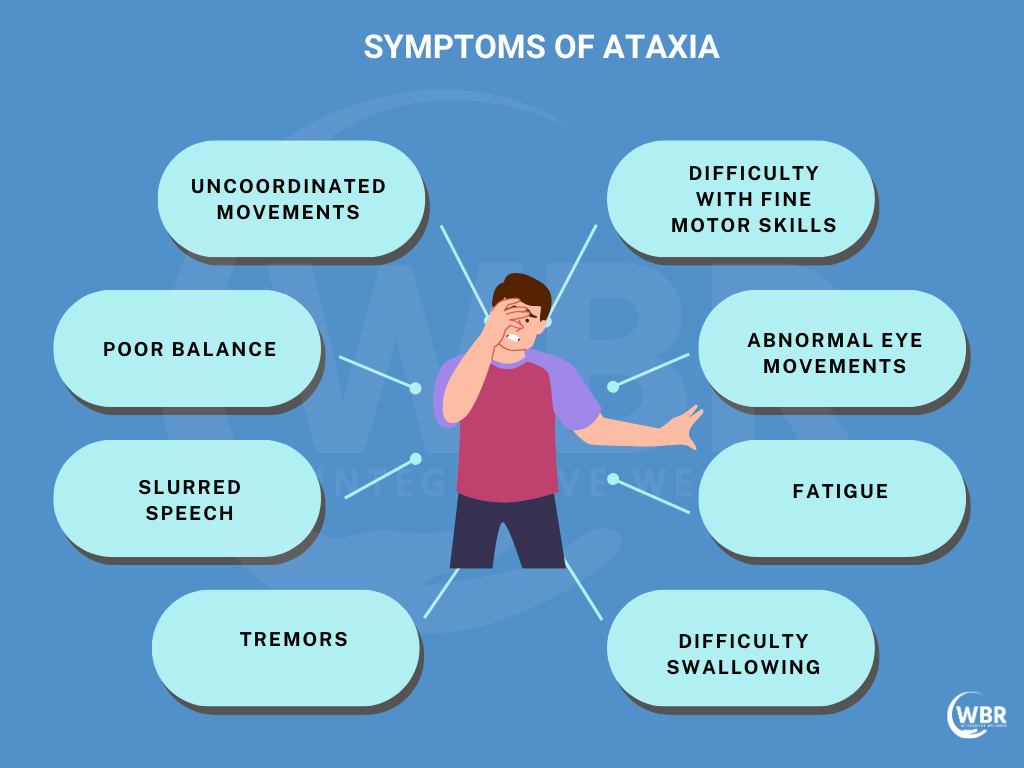
Symptoms of Ataxia
- Uncoordinated Movements: Difficulty with precise movements, such as picking up objects or walking in a straight line.
- Poor Balance: Frequent stumbling, trouble maintaining posture, and falls, especially when standing still or walking.
- Slurred Speech: Difficulty speaking clearly, often referred to as dysarthria, making communication challenging.
- Tremors: Shaking or tremors in hands, arms, or other body parts when attempting to perform tasks.
- Difficulty with Fine Motor Skills: Tasks like buttoning a shirt or writing become increasingly difficult.
- Abnormal Eye Movements: Rapid or uncontrolled eye movements (nystagmus) that affect vision and focus.
- Fatigue: Weakness and fatigue due to the increased effort required for basic tasks.
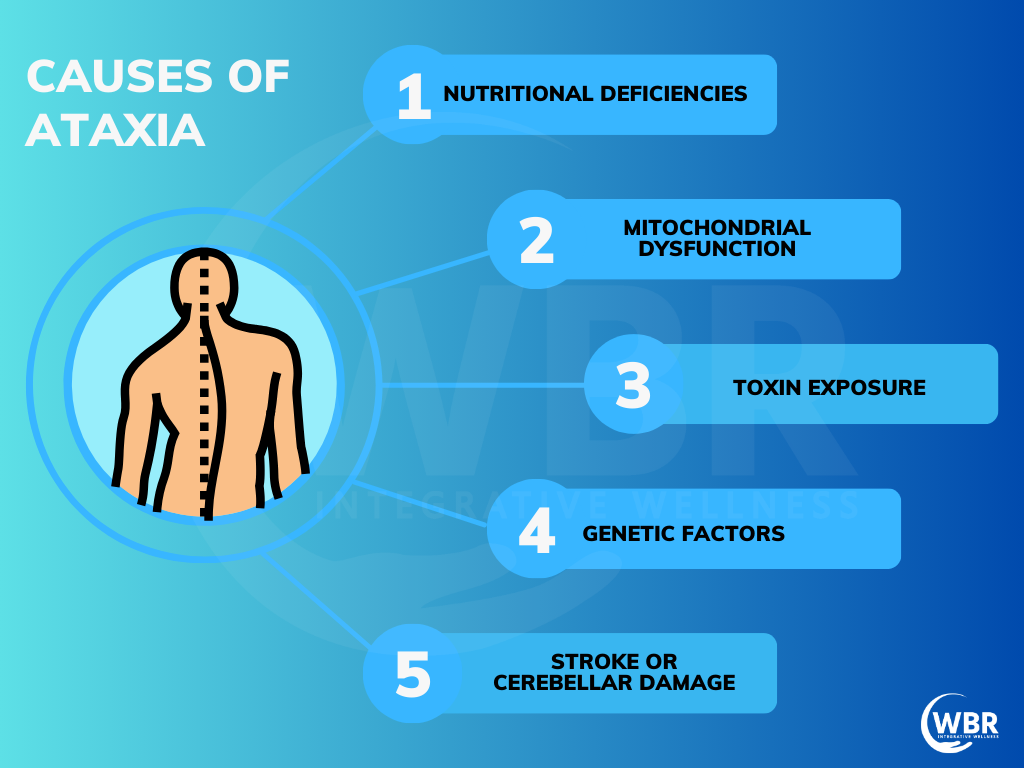
Common Causes of Ataxia
- Nutritional Deficiencies: Lack of key nutrients like thiamine (B1), vitamin B12, and vitamin E impair nerve function and coordination.
- Mitochondrial Dysfunction: Poor energy production in cells due to mitochondrial issues lead to muscle weakness and motor control problems.
- Toxin Exposure: Long-term exposure to heavy metals, alcohol, or environmental toxins damages the nervous system, resulting in ataxia.
- Genetic Factors: Inherited conditions such as Friedreich’s ataxia often cause progressive degeneration of the nervous system.
- Autoimmune Disorders: Conditions like multiple sclerosis or gluten ataxia trigger immune responses that damage the brain and nerves.
- Stroke or Cerebellar Damage: Injury to the cerebellum, which controls movement, is a common cause of ataxia.
Nutritional Deficiencies Linked to Ataxia
Thiamine (Vitamin B1) Deficiency: Thiamine is crucial for energy metabolism and maintaining nervous system health. A deficiency leads to nerve damage, causing symptoms like uncoordinated movement and muscle weakness.
Copper Deficiency: Copper is essential for proper nerve signaling. A lack of copper disrupts the nervous system, contributing to ataxia and related neurological issues.
Essential Fatty Acid Imbalance: Omega-3 and omega-6 fatty acids are vital for brain and nerve health. An imbalance leads to inflammation and impaired nerve function, worsening ataxia.
Vitamin B6, B12, and Vitamin E: These vitamins are key to preventing peripheral neuropathy and supporting healthy nerve function, which helps
Mitochondrial Health and Ataxia
Mitochondrial Dysfunction and Energy Production: Mitochondria are the “powerhouses” of cells, responsible for producing energy (ATP). When mitochondria don’t function properly, cells, particularly nerve cells, struggle to generate enough energy. This leads to muscle weakness, poor coordination, and the unsteady movements characteristic of ataxia.
Key Nutrients for Mitochondrial Function: Certain nutrients support mitochondrial health, including CoQ10, which aids energy production, and L-carnitine, which helps transport fatty acids into the mitochondria for energy conversion. Alpha-lipoic acid and B vitamins also play crucial roles.
Improving Mitochondrial Health: By enhancing mitochondrial function with these nutrients, individuals experience improved motor control, reduced fatigue, and better overall management of ataxia symptoms, as their cells regain energy efficiency.
Gut Health and Its Role in Ataxia
Gut-Brain Connection: The gut and brain are closely linked through the gut-brain axis, meaning gut health significantly impacts neurological function. Imbalances in gut flora contribute to neuroinflammation and worsening conditions like ataxia.
D-Lactate and Ataxia: When the gut ferments sugars inefficiently, it produces D-lactate, a type of lactic acid that the body struggles to detoxify. D-lactate accumulation leads to neurological issues such as confusion, cerebellar ataxia, and slurred speech.
Dietary Strategies: Reducing sugar and fruit intake helps minimize D-lactate production. A diet low in fermentable sugars, alongside probiotics to restore healthy gut bacteria supports both gut and brain health, alleviating some ataxia symptoms.
Gluten Sensitivity and Gluten Ataxia
Overview of Gluten Ataxia: Gluten ataxia is a neurological condition where the body’s immune response to gluten affects the brain, leading to motor coordination problems. This is associated with antibodies to specific transglutaminases—TG2 (found in the gut), TG3 (in the skin), and TG6 (in the brain).
Role of Transglutaminase Antibodies: The presence of these antibodies indicates an autoimmune reaction against gluten, which causes inflammation and damage in the brain, contributing to ataxia symptoms such as impaired coordination and balance.
How Gluten Sensitivity Triggers Neurological Symptoms: Gluten sensitivity leads to a breakdown of the blood-brain barrier, allowing immune cells to attack brain tissues. This immune reaction causes neurological symptoms like ataxia, confusion, and motor dysfunction.
Gluten-Free Dietary Recommendations: To manage gluten ataxia, it is crucial to follow a strict gluten-free diet. Avoiding all sources of gluten, including wheat, barley, and rye, helps reduce inflammation, prevent immune system activation, and improve neurological function.
Functional Medicine Approach to Ataxia
Root Cause Analysis: Functional medicine focuses on identifying underlying causes of ataxia, such as nutritional deficiencies (e.g., thiamine, copper), toxin exposure (e.g., heavy metals, alcohol), and mitochondrial dysfunction. This approach aims to understand how these factors contribute to the condition.
Personalized Treatment Plans: Based on the root causes identified, functional medicine practitioners create tailored treatment plans. These include dietary changes to address deficiencies, supplementation with essential nutrients (e.g., CoQ10, B vitamins), and detoxification strategies to eliminate toxins from the body.
Importance of Holistic Care: A holistic approach integrates nutrition, lifestyle changes (such as stress management and exercise), and medical support. This comprehensive care model not only targets the symptoms of ataxia but also improves overall health and well-being by addressing multiple aspects of the patient’s life.
Testing and Diagnostics
Diagnostic Tools for Identifying Ataxia Causes:
- Romberg Test: Evaluates balance by having the patient stand with feet together and eyes closed. Significant swaying indicates ataxia or related conditions.
- Blood Tests: Assess for nutritional deficiencies (e.g., thiamine, vitamin B12, copper), toxin levels (e.g., heavy metals), and inflammatory markers.
- Mitochondrial Function Tests: Measure indicators of mitochondrial health, such as CoQ10 levels and lactate levels, to evaluate energy production issues.
Functional Medicine Evaluations:
- Comprehensive Metabolic Panels: Evaluate overall metabolic health, including liver and kidney function.
- Genetic Testing: Identify genetic predispositions or mutations linked to ataxia.
- Gut Health Assessment: Analyze gut flora and D-lactate levels to address potential gut-brain connections.
- Customized Functional Assessments: Tailor evaluations to the individual’s specific symptoms and needs, guiding personalized treatment plans.
Nutritional and Lifestyle Strategies for Managing Ataxia
Dietary Modifications:
- Anti-Inflammatory Diet: Focus on foods that reduce inflammation, such as leafy greens, berries, and fatty fish. Avoid processed foods and excessive sugar.
- Nutrient-Dense Foods: Incorporate foods rich in essential nutrients, like nuts, seeds, and whole grains, to support overall health.
- Mitochondrial-Supporting Nutrients: Include foods high in CoQ10 (e.g., spinach, broccoli) and L-carnitine (e.g., red meat) to support cellular energy production.
Supplementation for Deficiencies:
- Thiamine and Copper: Supplement to address deficiencies that impair nerve function and coordination.
- Omega-3 Fatty Acids: Support brain health and reduce inflammation with supplements or foods like flaxseeds and fish oil.
- CoQ10: Enhance mitochondrial function and energy production with CoQ10 supplements.
Lifestyle Practices:
- Stress Management: Practice relaxation techniques such as meditation or yoga to reduce stress, which exacerbate ataxia symptoms.
- Quality Sleep: Ensure adequate and restful sleep to support overall neurological and physical health.
- Regular Physical Therapy: Engage in physical therapy to improve motor coordination, balance, and overall mobility.
Conclusion
Addressing ataxia effectively requires a comprehensive approach that integrates nutritional and functional medicine. By identifying and correcting underlying causes—such as nutritional deficiencies, mitochondrial dysfunction, and toxin exposure—patients experience significant improvements in symptoms. A personalized treatment plan, encompassing dietary modifications, targeted supplementation, and lifestyle changes, plays a crucial role in managing ataxia.