A Comprehensive Guide to Chronic Diarrhoea: An Integrative Approach
Chronic diarrhoea affects up to 5% of the global population at any given time, disrupting daily life and often signaling deeper health imbalances. Defined as loose stools lasting over four weeks, it stems from infections, gut inflammation, IBS, food intolerances, or systemic disorders. With more than 100 possible causes, finding lasting relief is challenging. In this blog, a Comprehensive Guide to Chronic Diarrhoea: An Integrative Approach, we have combined the precision of conventional diagnostics with the root-cause lens of functional medicine to offer clinicians and patients a complete, actionable roadmap for healing, one that addresses both symptoms and the systems driving them.
Classification of Chronic Diarrhoea
Classification of Chronic Diarrhoea
Identifying the type of chronic diarrhoea is essential to uncover its root cause. Here’s a quick breakdown:
- Secretory Diarrhea: It is caused by excess water and electrolyte secretion and is unaffected by fasting.
Common causes: Bile acid malabsorption, hormone-secreting tumors, SSRIs, and microscopic colitis. - Osmotic Diarrhoea: It is triggered by non-absorbable substances drawing water into the gut.
Common causes: Lactose intolerance, sugar alcohols, laxative abuse. Clue: Resolves with fasting. - Inflammatory Diarrhoea: Here, mucosal damage causes blood, mucus, and protein leakage.
Common causes: IBD, infections, radiation enteritis. - Fatty Diarrhoea (Steatorrhoea): In this type of diarrhoea, fat malabsorption results in oily, bulky stools.
Common causes: Pancreatic insufficiency, celiac disease, SIBO. - Functional Diarrhoea: Linked to IBS-D and gut-brain axis dysfunction, often with dysbiosis.
Causes of Chronic Diarrhoea
Chronic diarrhoea has a wide range of potential causes that are grouped into gastrointestinal, systemic, medication-related, and post-surgical categories:
Gastrointestinal Causes
- Inflammatory: Conditions like Inflammatory Bowel Disease (IBD – Crohn’s disease, Ulcerative Colitis) and microscopic colitis cause mucosal inflammation leading to persistent diarrhoea.
- Infectious: Chronic diarrhoea follows infections (Post-infectious IBS) or result from parasites (e.g., Giardia) and bacteria like Yersinia and Campylobacter.
- Malabsorption Syndromes: Conditions such as celiac disease and tropical sprue impair nutrient absorption, especially fats, causing steatorrhea.
- Motility Disorders: IBS with diarrhoea (IBS-D) and post-cholecystectomy syndrome can increase gut motility, contributing to loose stools.
- Anatomic Changes: Surgeries causing short bowel syndrome or altering gut structure can lead to chronic diarrhoea due to decreased absorption.
Systemic Diseases
- Endocrine/Metabolic: Hyperthyroidism and Addison’s disease affect fluid balance.
- Neurological/Autoimmune: Diabetes (via autonomic neuropathy) and scleroderma impair GI function.
Medication-Induced
- Drugs such as metformin, magnesium-containing antacids, certain antibiotics (e.g., clindamycin → C. difficile), and chemotherapeutics commonly trigger chronic diarrhoea.
Post-Surgical Conditions
- Procedures like small bowel resection, cholecystectomy, or vagal nerve injury disrupt digestion and absorption, leading to chronic diarrhoea.
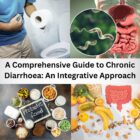
What is Chronic Dirrhoea?
Chronic diarrhoea is defined as the passage of loose, watery, or frequent stools, typically three or more times a day, persisting for over four weeks. Unlike acute diarrhoea, which is usually caused by infections and resolves within days, chronic diarrhoea indicates an ongoing disruption in gut function or an underlying health condition. It is often accompanied by bloating, urgency, abdominal pain, or unintended weight loss. The causes of chronic diarrhoea range from irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) to malabsorption issues, chronic infections, and medication side effects. Understanding the duration, frequency, and associated symptoms is key to narrowing down its root cause.
Functional Medicine Lens: Root-Cause Exploration
Functional medicine aims to understand why chronic diarrhoea is happening by investigating the underlying imbalances and systemic dysfunctions that conventional approaches often overlook. Here are five key areas of exploration:
- Gut Microbiome Imbalance (Dysbiosis)
Disruption of the gut microbial ecosystem due to antibiotics, poor diet, chronic stress, or infections drive chronic diarrhoea.
- Testing: GI-MAP, organic acids, comprehensive stool analysis
- Treatment: Probiotics, prebiotics, fermented foods, and targeted herbal antimicrobials
- Small Intestinal Bacterial Overgrowth (SIBO) and Intestinal Methanogen Overgrowth (IMO)
An overgrowth of microbes in the small intestine cause bloating, gas, and diarrhoea or constipation.
- Diagnosis: Lactulose/mannitol breath test
- Treatment: Herbal antimicrobials, elemental diet, motility agents like ginger or low-dose erythromycin
- Food Sensitivities and Intolerances
Certain foods trigger immune or non-immune responses leading to GI symptoms.
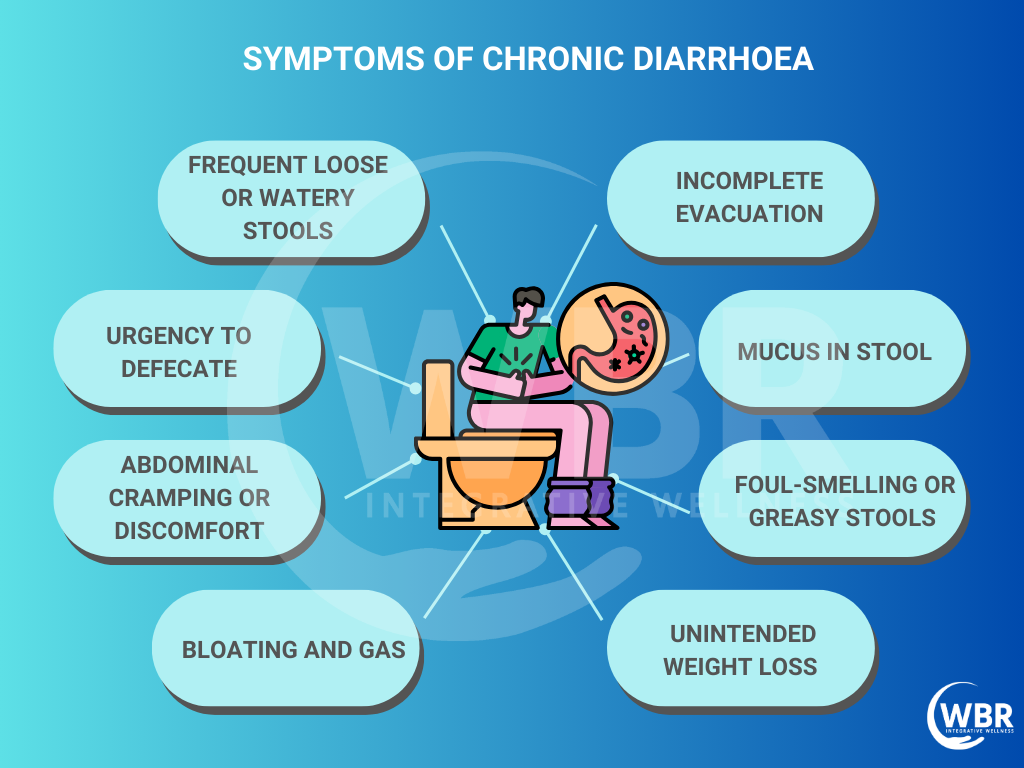
- Common triggers: Gluten, dairy, FODMAPs, eggs
- Tools: Elimination diets, MRT (Mediator Release Testing)
- Approach: Tailored dietary modification to reduce inflammation
- Impaired Digestive Function
Low stomach acid, poor enzyme output, or sluggish bile flow hinder digestion and cause diarrhoea.
- Support: Betaine HCl, digestive enzymes, and ox bile supplements
- Intestinal Permeability (Leaky Gut)
Damage to the intestinal lining allows unwanted particles into circulation, triggering inflammation.
- Triggers: Gluten, NSAIDs, alcohol, stress
- Tests: Zonulin levels, lactulose/mannitol permeability challenge
- Restoration: L-glutamine, zinc carnosine, quercetin, colostrum
By addressing these root causes, functional medicine provides a holistic path to long-term relief.
Diagnostic Approach
A thorough and systematic evaluation is crucial for diagnosing the root cause of chronic diarrhoea. Functional and conventional tools work synergistically to uncover hidden imbalances.
Initial Evaluation
Begin with a detailed history focusing on onset, duration, stool characteristics, dietary triggers, recent travel, infections, and medication use (e.g., antibiotics, laxatives).
- Physical exam: Assess hydration status, signs of malnutrition, abdominal tenderness, and unintentional weight loss.
Laboratory Tests
Baseline labs help detect inflammation, infection, and systemic conditions:
- CBC, CRP, ESR: Identify anemia, systemic or gut inflammation
- TSH, fasting glucose, cortisol: Rule out endocrine causes (e.g., hyperthyroidism, diabetes, Addison’s)
- Liver function tests, vitamin B12, folate: Check for malabsorption and liver-related diarrhoea
- Fecal markers: Calprotectin or lactoferrin for inflammation
- Stool tests: Assess for white blood cells, fat content, ova/parasites, and bacterial culture
Imaging & Endoscopy
- Colonoscopy with biopsy: Essential to evaluate for IBD, microscopic colitis, and malignancies
- Upper endoscopy with duodenal biopsy: Helps confirm celiac disease
- CT or MRI abdomen: Useful for detecting masses, lymphadenopathy, or anatomical changes
Functional Tests
- SIBO breath test: Detects bacterial overgrowth in the small intestine
- Stool zonulin: Marker for intestinal permeability (leaky gut)
- GI pathogen DNA panels: Identify low-grade or chronic infections
- Comprehensive stool testing (e.g., GI360, GI-MAP): Evaluate microbiome diversity, inflammation, digestion, and infection
Together, these tools provide a comprehensive roadmap for diagnosing and treating chronic diarrhoea effectively.
Functional and Nutritional Interventions
In functional medicine, diet and targeted nutrients play a pivotal role in managing chronic diarrhoea by supporting gut healing and reducing inflammation. These interventions aim not just to relieve symptoms but to restore optimal gastrointestinal function.
- Dietary Modifications: Begin with eliminating common triggers through a low-FODMAP, gluten-free, or dairy-free diet. In more complex cases, the Specific Carbohydrate Diet (SCD) or Autoimmune Paleo (AIP) may be beneficial.
- Gut-Healing Nutrients:
- L-glutamine: Fuels intestinal cells and supports barrier integrity
- Zinc carnosine: Promotes mucosal healing
- Omega-3 fatty acids: Reduce gut inflammation
Aloe vera, slippery elm, marshmallow root: Soothe and protect the gut lining
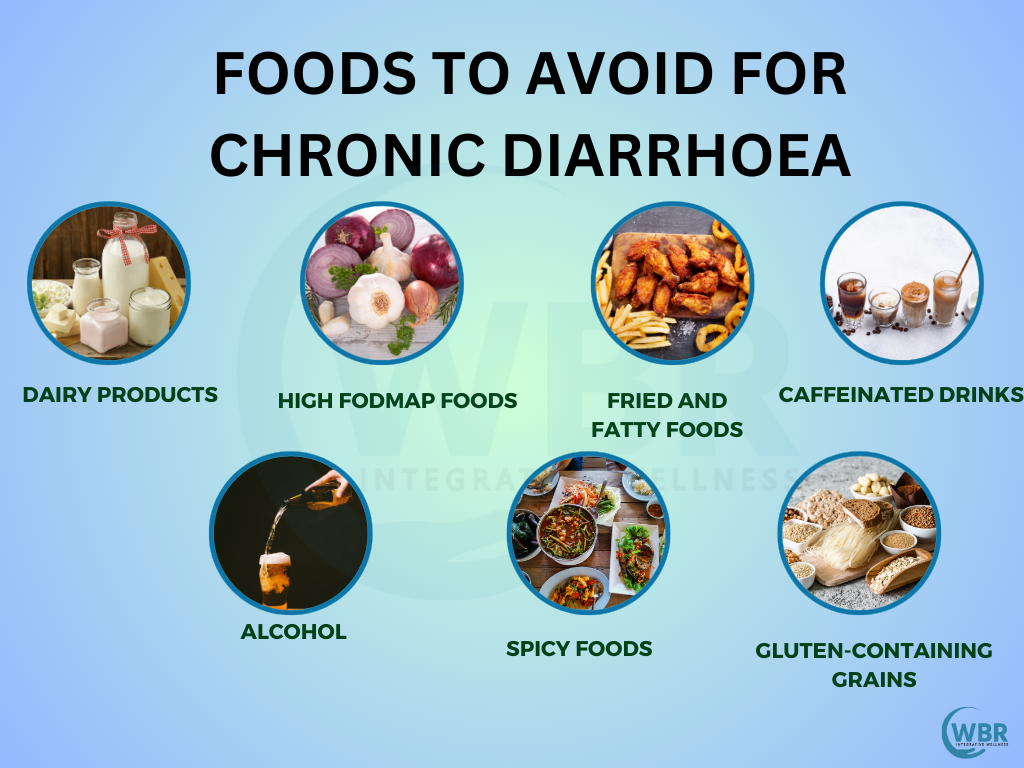
Microbiome Support
Maintaining a healthy and diverse gut microbiome is central to the integrative management of chronic diarrhoea. Dysbiosis or an imbalance of gut bacteria impair digestion, increase inflammation, and compromise intestinal barrier function. Targeted microbiome support helps restore balance, alleviate symptoms, and support long-term gut health.
- Probiotics: Use evidence-based, multi-strain formulations tailored to individual needs. Key strains shown to support gut health and reduce diarrhoea include:
- Lactobacillus rhamnosus GG (LGG) – Effective in antibiotic-associated and infectious diarrhoea
- Saccharomyces boulardii – A beneficial yeast particularly helpful in traveller’s diarrhoea and C. difficile prevention
- Bifidobacterium longum – Supports immune function and reduces inflammation
- Lactobacillus plantarum and L. acidophilus – Aid in gut barrier integrity and reduce IBS symptoms
These probiotics help re-establish beneficial bacteria, modulate immune responses, and restore microbial diversity.
- Prebiotics: Fibres such as inulin, fructooligosaccharides (FOS), and galactooligosaccharides (GOS) selectively feed beneficial bacteria like Bifidobacteria. However, in patients with diarrhoea or SIBO. Prebiotics should be introduced gradually and monitored closely, as they ofteb temporarily increase bloating or loose stools.
- Polyphenols: Naturally occurring plant compounds found in green tea, blueberries, pomegranate, turmeric, and cocoa help modulate the microbiota. They encourage the growth of beneficial bacteria like Akkermansia muciniphila and Faecalibacterium prausnitzii, while reducing pathogenic species. Additionally, polyphenols possess anti-inflammatory, antioxidant, and gut-barrier-protective effects.
Together, probiotics, prebiotics, and polyphenols provide a comprehensive, functional approach to rebuilding a resilient gut ecosystem in chronic diarrhoea.
Stress Modulation
Chronic stress and cortisol dysregulation significantly impact gut health by altering motility, increasing intestinal permeability (leaky gut), and disrupting the microbiome. Stress is a known trigger and exacerbator of functional diarrhoea, particularly in IBS-D. Addressing the gut-brain connection is, therefore, crucial in a holistic approach.
Mind-body interventions such as meditation, deep breathing, yoga, and guided imagery help regulate the stress response and improve GI symptoms. Additionally, adaptogenic herbs like ashwagandha and rhodiola support adrenal function and balance cortisol levels, promoting resilience and gut healing. Stress reduction is a vital yet often overlooked pillar of long-term recovery.
Red Flags Needing Urgent Evaluation
While many cases of chronic diarrhoea are benign or functional, certain symptoms signal the need for immediate and thorough investigation to rule out serious underlying conditions:
- Blood in stool – It indicates IBD, colorectal cancer, or infection
- Unintentional weight loss – Suggests malabsorption, malignancy, or chronic inflammation
- Nocturnal diarrhoea – Often points to organic rather than functional causes
- Family history of colon cancer – Increases risk for malignancy
- Recent travel with fever – Could indicate parasitic or bacterial infection
- Age >50 with new-onset diarrhoea – Warrants colonoscopy to exclude colorectal cancer or other pathology
Special Considerations
Elderly: More prone to chronic diarrhoea due to medications (e.g., laxatives, antibiotics), pancreatic insufficiency, or bile acid malabsorption. A comprehensive medication review is essential.
Children: Common causes include coeliac disease, post-infectious diarrhoea, and food allergies. Growth monitoring and dietary assessment are crucial for early intervention.
Immunocompromised: Higher risk for infections like CMV, Cryptosporidium, and MAC. Prompt stool testing and tailored antimicrobial treatment are vital to prevent severe complications.
Summary Checklist for Clinicians
A structured, integrative approach helps clinicians manage chronic diarrhoea effectively:
- Classify the diarrhoea subtype: Secretory, osmotic, inflammatory, fatty, or functional
- Rule out red flags: Blood in stool, weight loss, nocturnal symptoms, age >50
- Order targeted investigations: Labs, endoscopy, imaging as needed
- Use stool and breath tests: Evaluate for SIBO, infections, malabsorption
- Identify triggers: Food sensitivities, stress, medications, travel
- Address gut dysbiosis: Probiotics, prebiotics, antimicrobials, healing nutrients
- Patient education: Support long-term lifestyle and dietary modifications for sustained gut health
Conclusion
Chronic diarrhoea requires more than symptom control. It calls for a dual-lens approach that addresses both overt disease and subtle imbalances like dysbiosis, food sensitivities, and poor digestion. By combining conventional diagnostics with functional, root-cause interventions, clinicians can uncover hidden drivers and create personalized, sustainable treatment plans. This integrative strategy empowers patients on their path to lasting relief and resilient gut health.