Functional Medicine Approach for Eczema
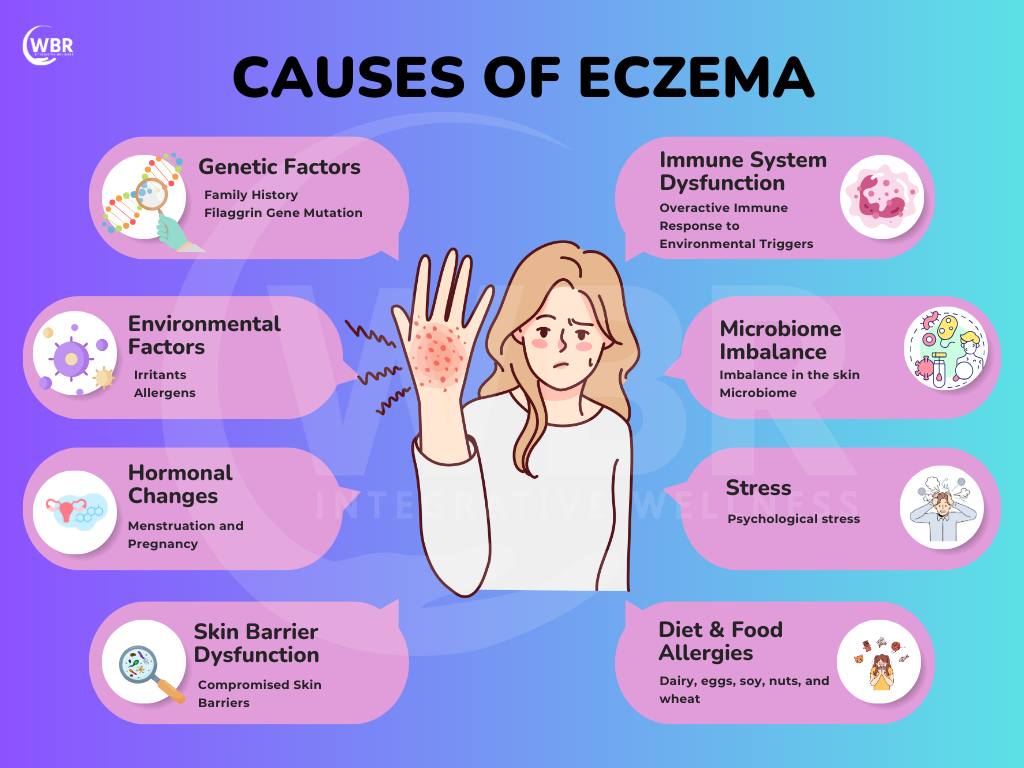
Eczema, a common itchy skin condition, affects up to 20% of the population, particularly children, and is often associated with hay fever and asthma. It often persists into adulthood, with sufferers relying on a range of treatments, from pharmaceutical steroids to herbal remedies, to manage symptoms. However, many find these treatments lose effectiveness over time, as they don’t address the root cause—a bacterial infection caused by Staphylococcus aureus. This bacterium, commonly found on eczema-prone skin, exacerbates the condition by hindering the absorption of topical treatments like hydrocortisone. Studies show that up to 80% of eczema sufferers have underlying food sensitivities or imbalances in their gut microbiome. A personalized, holistic approach not only alleviates symptoms but also reduces the likelihood of flare-ups in the long term. In this blog, we’ll explore how functional medicine offers a comprehensive, effective strategy for managing and potentially overcoming eczema.
Understanding Eczema
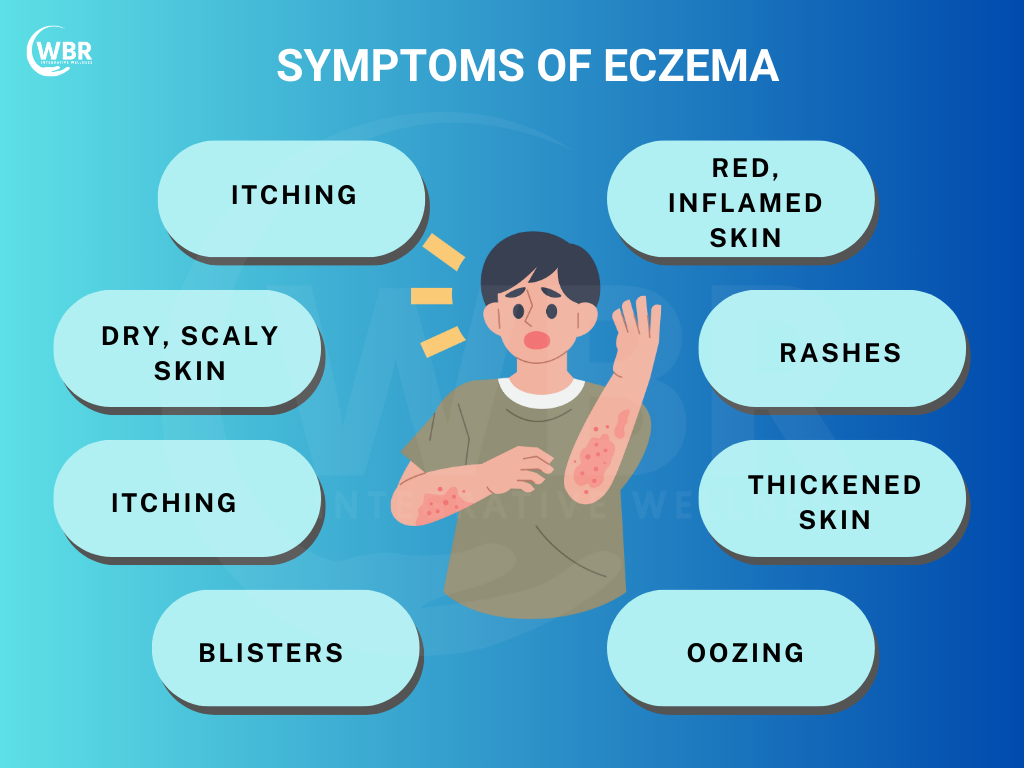
Eczema is a chronic skin condition characterized by inflammation, redness, and itching. Among its various forms, Atopic Dermatitis (AD) is the most common, affecting millions worldwide. AD typically begins in childhood and is marked by recurring episodes of itchy, inflamed skin, often on the face, hands, and behind the knees. What sets AD apart is its strong connection to a personal or family history of allergic conditions such as asthma, hay fever, or food allergies. In fact, up to 70% of those with Atopic Dermatitis have a family history of these allergic conditions. The prevalence of Atopic Dermatitis is rising, particularly in urban and developed areas, affecting up to 20% of children and 3% of adults globally. Understanding this link between AD and allergic conditions is crucial for effective management and treatment, making it clear that eczema is not just a skin condition but a complex immune response.
Types of Eczema and Their Characteristics
Eczema is an inflammatory skin condition that causes redness, itching, and irritation. While all types share common symptoms, their triggers and underlying causes vary. Understanding the different types of eczema helps in effective management and treatment.
- Contact Eczema (Contact Dermatitis): This type occurs when the skin reacts to allergens or irritants like detergents, fragrances, or metals. Symptoms include redness, itching, and sometimes blisters, appearing only in the exposed area. Avoiding triggers and using soothing creams can help manage flare-ups.
- Atopic Eczema (Atopic Dermatitis): Atopic eczema is a chronic condition linked to an overactive immune system, often running in families with allergies or asthma. It causes dry, itchy, and inflamed skin, worsened by environmental triggers like dust and pollen. Hydration and anti-inflammatory treatments help control symptoms.
- Seborrheic Eczema (Seborrheic Dermatitis): This type mainly affects oily areas like the scalp, face, and chest due to an overgrowth of yeast. It presents as greasy, yellowish flakes with redness and itching. Antifungal treatments and mild medicated shampoos are commonly used for relief.
- Nummular Eczema (Discoid Eczema): Nummular eczema appears as round, scaly patches, often triggered by dry skin, cold weather, or skin injuries. It can be intensely itchy and sometimes mistaken for fungal infections. Regular moisturization and topical steroids help with the treatment.
- Stasis Eczema (Venous Eczema): Caused by poor blood circulation, stasis eczema affects the lower legs, leading to swelling, redness, and itching. Over time, the skin may thicken and develop sores. Elevating the legs, compression therapy, and improving circulation can help manage it.
- Neurodermatitis: Triggered by stress and habitual scratching, neurodermatitis causes thickened, leathery patches of skin. It commonly appears on the neck, wrists, or ankles and worsens with continued scratching. Stress management and topical medications are essential for relief.
Gut and Skin Microbiota in Eczema
Skin Dysbiosis and Its Impact
Skin dysbiosis refers to an imbalance in the skin’s microbial community, often marked by the overgrowth of harmful bacteria like Staphylococcus aureus. This imbalance exacerbates eczema by promoting inflammation and disrupting the skin barrier. Staphylococcus aureus produces toxins that aggravate eczema symptoms, leading to increased redness, itching, and inflammation. Additionally, yeast and fungi, such as Malassezia, also contribute to skin inflammation, further complicating eczema management.
Gut Dysbiosis and Eczema
Gut dysbiosis, an imbalance in the gut microbiota, is linked to eczema exacerbation. Overgrowth of bacteria like Clostridium difficile and an imbalance between beneficial and harmful gut bacteria influence systemic inflammation and immune responses. Furthermore, this disruption manifests as worsening eczema symptoms, as the gut microbiome plays a crucial role in modulating skin inflammation and immune function.
Managing Eczema Through Microbiota
Addressing microbiota imbalances offers the potential for managing eczema. Moreover, probiotic supplements can restore a healthy balance in both gut and skin microbiota, potentially reducing inflammation and improving skin health. Dietary interventions that promote gut health, such as consuming prebiotic-rich foods, support this balance. Ensuring a healthy gut microbiome leads to improved eczema symptoms and overall skin condition.
Core Treatment Goals in the Functional Medicine Approach for Eczema
The functional medicine approach targets the root causes of eczema by strengthening the skin barrier, regulating the immune system, and supporting gut health.
- Strengthening Skin Barrier Integrity – Nourishing the skin with essential fatty acids, ceramides, and natural moisturizers helps protect against irritants and infections.
- Regulating Immune Response – Identifying triggers, reducing inflammation with omega-3s and vitamin D, and balancing immune function help prevent flare-ups.
- Supporting Gut Health – Healing the gut with probiotics, fiber-rich foods, and addressing imbalances improves immune tolerance and reduces skin inflammation.
Dietary Factors in Eczema Management
Diet plays a pivotal role in managing eczema, particularly for those with Atopic Dermatitis (AD). One significant aspect is the impact of food allergies. Common allergens such as eggs, milk, wheat, and soy are linked to eczema flare-ups, especially in children. While the evidence on the direct impact of these allergens is mixed, many individuals report symptom improvement through elimination diets. By systematically removing and reintroducing suspected allergens, individuals must identify specific triggers and potentially alleviate eczema symptoms.
Nickel sensitivity is one such dietary consideration for managing Eczema. Nickel, found in foods like nuts, chocolate, and certain legumes exacerbates eczema in sensitive individuals. Thus, reducing the intake of nickel-rich foods offers relief for some patients, highlighting the need for personalized dietary approaches.
Sodium intake also influences eczema management. High sodium levels contribute to skin dryness and exacerbate symptoms. Reducing sodium intake by cutting back on processed foods and opting for fresh, whole foods helps improve skin hydration and reduce flare-ups.
Trans fatty acids, commonly found in processed and fried foods, are associated with increased inflammation and worsening eczema. Hence, avoiding trans fats and focusing on a diet rich in healthy fats, such as those from avocados, nuts, and olive oil support overall skin health and potentially reduce AD symptoms.
Lifestyle and Dietary Strategies for Eczema
A holistic approach to eczema includes diet, stress management, and mindful skincare to reduce flare-ups and support healing.
- Anti-Inflammatory Diet – Focus on whole foods like fruits, vegetables, and healthy fats while avoiding processed foods, dairy, and excessive sugars that can trigger inflammation.
- Fermented Foods – Foods like yogurt, kimchi, and sauerkraut provide probiotics that help balance the gut microbiome, supporting immune function and skin health.
- Stress Management – Practices like yoga, meditation, and mindfulness reduce stress-related flare-ups by regulating cortisol and calming the nervous system.
- Avoiding Harsh Chemicals – Switching to fragrance-free, hypoallergenic skin and household products minimizes irritation and preserves the skin’s protective barrier.
Nutritional and Supplement Support for Eczema
Targeted nutrition and supplements help reduce inflammation, support immune balance, and promote skin healing in eczema.
- Omega-3 Fatty Acids – Found in fish oil and flaxseeds, omega-3s help reduce inflammatory pathways and support skin hydration.
- Vitamin D – Essential for immune regulation and skin integrity, adequate levels help prevent flare-ups.
- Probiotics & Prebiotics – Strengthen gut microbiome balance, enhancing immune tolerance and reducing eczema severity.
- Quercetin & Bromelain – These natural compounds act as antihistamines and anti-inflammatories, easing allergic reactions.
- Zinc & Vitamin C – Support wound healing, collagen formation, and immune defense against skin infections.
- Herbs for Detoxification – Milk Thistle, Green Tea, and Reishi Mushrooms aid liver
The Role of Probiotics and Prebiotics in Managing Eczema
When considering probiotics and prebiotics for eczema, it’s essential to focus on specific strains and types that have shown promise in research.
Probiotics
- Lactobacillus rhamnosus GG: One of the most studied strains, this probiotic has shown potential in reducing eczema symptoms, especially in children. It helps improve the skin barrier and modulate the immune system.
- Bifidobacterium lactis: This strain is known for its beneficial effects on gut health and is associated with reduced eczema symptoms in some studies.
- Lactobacillus fermentum: Some research suggests that this strain helps improve eczema symptoms by supporting the skin’s natural defenses.
- Lactobacillus acidophilus: Often used in combination with other probiotics, it helps in balancing the gut microbiome, potentially impacting eczema.
Prebiotics
- Inulin: A type of soluble fiber that acts as a food source for beneficial gut bacteria. It helps improve gut health and indirectly benefit skin conditions.
- Fructooligosaccharides (FOS): Found in various fruits and vegetables, FOS supports the growth of beneficial bacteria in the gut.
- Galactooligosaccharides (GOS): These prebiotics are found in certain dairy products and are linked to improved gut health and immune function.
- Beta-glucans: Found in oats and barley, beta-glucans have immune-modulating effects and support overall gut health.
Tips for Use
- Quality Matters: Choose high-quality probiotic supplements with well-documented strains and adequate CFUs (colony-forming units).
- Consult a Healthcare Professional: It’s crucial to discuss with a healthcare provider before starting any new probiotic or prebiotic regimen, especially for managing eczema.
- Dietary Sources: Incorporating probiotic-rich foods (like yogurt and kefir) and prebiotic-rich foods (such as bananas, onions, and garlic) into your diet is beneficial.
While these probiotics and prebiotics offer benefits, they should be part of a broader eczema management plan, including proper skin care and avoiding known triggers.
Lifestyle Changes and Additional Treatments for Eczema
Functional Medicine Treatments:
- Anti-inflammatory Supplements: Omega-3s, vitamin D, zinc, and probiotics support skin health and reduce inflammation.
- Antihistamine Compounds: Quercetin helps control histamine-related symptoms.
- Allicin: A potent agent proven to kill Staphylococcus aureus and promote healing, offering a breakthrough for eczema sufferers both as caps at dose of 1200 to 1800 mg for a month and tropical application of allicin gel or cream as option.
- Working to resolve SIBO, SIFO and working on GUT lining repair.
Lifestyle Adjustments for Eczema Management:
- Improve Sleep: Quality sleep helps manage symptoms and support overall health.
- Reduce Toxin Exposure: Minimize contact with irritants and environmental toxins.
- Consider Phototherapy: Controlled UV light therapy can help reduce inflammation.
- Mindfulness and Stress Reduction: Techniques like meditation and yoga reduce stress, which can trigger flare-ups.
Additional Dietary and Supplement Recommendations:
- Avoid High-Histamine Foods: Reducing intake may prevent flare-ups.
- Supplement with Flaxseed Oil: Rich in omega-3s to support skin health.
- Melatonin: May improve sleep quality and reduce eczema severity in children.
- Gastric Acid Replacement Therapy: Can be beneficial for some, aiding in digestion and potentially reducing flare-ups.
- Avoid Fluoride in Toothpaste: Some individuals may find relief by using fluoride-free products.
Testing and Diagnosis for Eczema
Accurate testing helps identify triggers and underlying imbalances contributing to eczema flare-ups.
- Food Sensitivity Tests – Detects specific food intolerances, such as dairy, gluten, or nuts, that may be exacerbating inflammation and skin reactions.
- Omega-3 Index Test – Measures the balance of omega-3 and omega-6 fatty acids, providing insight into systemic inflammation and the need for dietary adjustments.
- Patch Testing – Identifies contact allergens like fragrances, metals, or chemicals that may be triggering eczema, guiding personalized skincare and lifestyle changes.
Prevention and Early Intervention for Eczema
Prevention and Early Intervention
Breastfeeding and Maternal Diet:
- Breastfeeding Duration: Breastfeeding for over six months significantly reduces the risk of eczema in high-risk infants, providing essential nutrients and immune system support.
- Maternal Diet: The mother’s diet during breastfeeding plays a role in influencing the child’s eczema risk. Furthermore, avoiding allergenic foods such as dairy, peanuts, and shellfish decreases the likelihood of eczema development in the infant. A balanced, allergy-conscious diet helps in reducing the infant’s exposure to potential allergens.
Black Currant Seed Oil (BCSO) Study Overview:
- Study Summary: Research has shown that supplementing with Black Currant Seed Oil (BCSO) during pregnancy and early childhood is associated with a lower prevalence of eczema at 1 and 2 years of age. BCSO, rich in gamma-linolenic acid, helps in modulating inflammation and supporting skin health.
- Implications for Early Intervention: These findings suggest that BCSO supplementation could be a promising strategy for early eczema prevention. Incorporating BCSO into maternal and infant care routines provides additional support in reducing eczema risk and promoting overall skin health from a young age.
Conclusion
Effective eczema management combines conventional treatments with lifestyle and dietary adjustments. Utilizing emollients, antihistamines, and biologics, alongside anti-inflammatory supplements and stress reduction techniques, significantly alleviates symptoms. Dietary strategies, like avoiding high-histamine foods and supplementing with beneficial oils, along with early interventions such as extended breastfeeding and BCSO, offer promising prevention and management avenues. A holistic approach addressing both symptoms and underlying factors is key to improving eczema control and overall quality of life.