Functional Medicine Approach for Diverticulosis & Diverticulitis
Diverticulosis and diverticulitis are increasingly common digestive conditions, particularly in Western societies, where a low-fiber diet is prevalent. Diverticulosis, characterized by small pouches (diverticula) that form in the colon, affects approximately 20% of individuals aged 40-49. It rises sharply to 75% in those over 80. While diverticulosis is often asymptomatic, about 5% of individuals with diverticulitis will develop diverticulitis. This condition reflects the impact of modern dietary habits on gut health. Evidence suggests a direct correlation between low dietary fiber intake and the development of diverticular disease. In regions where high-fiber diets are the norm, such as in certain parts of Africa, diverticular disease is virtually nonexistent. Understanding the root causes and preventive strategies is crucial for managing these conditions and improving overall digestive health.
What is Diverticulosis?
Diverticulosis is a condition that results in the formation of small, bulging pouches called diverticula in the walls of the colon. These pouches develop when weak spots in the muscle layer of the colon give way under pressure, often due to straining during bowel movements. Moreover, this condition is largely asymptomatic. Many people have diverticula without experiencing any noticeable symptoms. However, when symptoms do occur, they typically include mild abdominal discomfort, bloating, and changes in bowel habits, such as constipation or diarrhea. The primary cause of diverticulosis is believed to be a diet low in fiber. A low-fiber diet leads to harder stools and increased pressure in the colon during bowel movements.
Prevalence of Diverticulosis
The condition’s prevalence is so widespread that by the age of 60, more than half of the population in developed nations have some degree of diverticulosis. Interestingly, diverticulosis is rare in countries where people consume diets rich in fiber, highlighting the role that diet plays in the development of this condition.
Symptoms of Diverticulosis
Most individuals with diverticulosis do not experience symptoms, making the condition difficult to detect without medical imaging. However, when symptoms do occur, they are generally mild.

Risk Factors for Diverticulosis
Several factors increase the likelihood of developing diverticulosis:
- Low-Fiber Diet: Diets lacking in fiber are strongly linked to the formation of diverticula. Fiber helps to soften stools, making them easier to pass and reducing pressure on the colon walls.
- Aging: As people age, the colon walls weaken, making them more susceptible to diverticula formation. Even though the condition is rare before the age of 40, it becomes much more common as people age.
- Genetics: A family history of diverticulosis increases the risk, suggesting a hereditary component to the condition.
- Sedentary Lifestyle: Physical inactivity slows down digestion and leads to constipation, increasing the risk of diverticulosis.
- Obesity: Higher body weight increases abdominal pressure, contributing to the formation of diverticula.
- Smoking: Smoking leads to an increased risk of diverticulosis, possibly due to its impact on blood circulation and tissue health.
- Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids, increase th
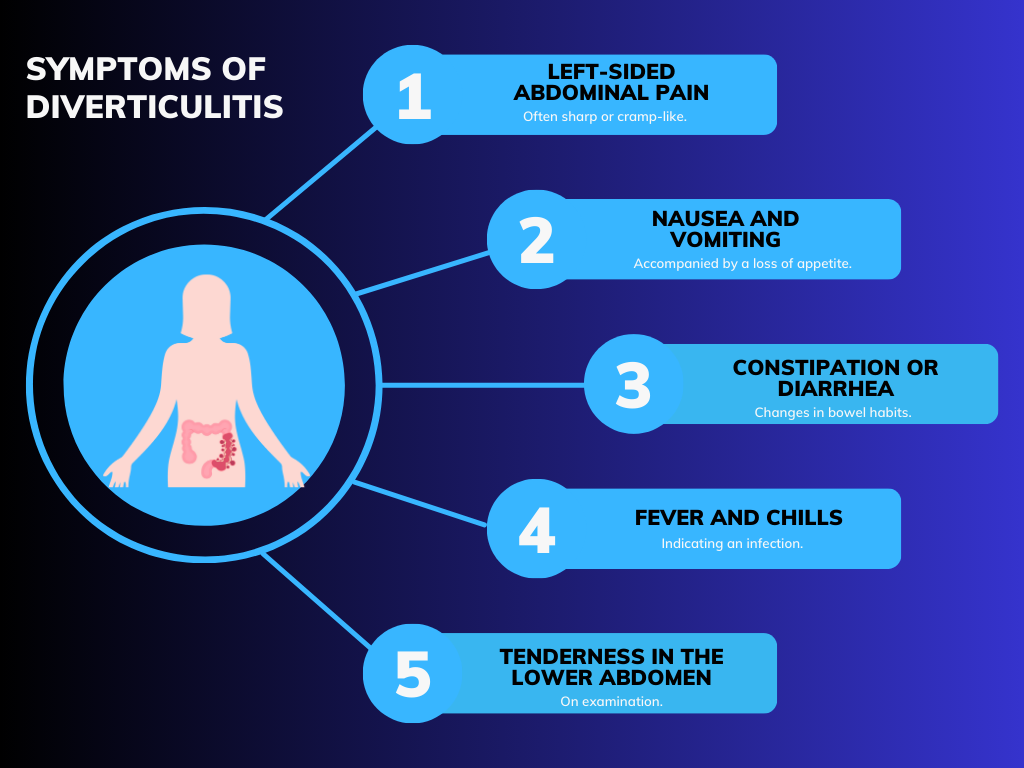
What is Diverticulitis?
Diverticulitis is a condition that arises when diverticula—small, bulging pouches formed in the walls of the colon—become inflamed or infected. This inflammation leads to severe abdominal pain and other complications. Unlike diverticulosis, which often has no symptoms, diverticulitis presents more acute and severe health issues. The inflammation causes the walls of the colon to thicken and leads to the formation of abscesses, fistulas, or even bowel obstructions. The condition often requires medical treatment, which includes antibiotics, dietary changes, or in severe cases, surgery.
Risk Factors for Diverticulitis
- Low-fiber diet: Contributing to constipation and increased pressure in the colon.
- Age: Risk increases with age, especially over 50.
- Obesity: Excess weight can exacerbate colon issues.
- Sedentary lifestyle: Lack of physical activity can worsen symptoms.
- Smoking: Associated with an increased risk of diverticulitis.
- Certain medications: Such as non-steroidal anti-inflammatory drugs (NSAIDs) and steroids.
These risk factors overlap with those for diverticulosis but become more significant when diverticulitis develops due to the added complications of inflammation and infection.
Dietary Recommendations Tips for Diverticulosis and Diverticulitis
- During Flares: Focus on a Clear Liquid Diet
- Clear Liquid Diet: During an acute flare of diverticulitis, it’s essential to rest the digestive system. Thus, a clear liquid diet, which includes water, broth, and clear juices, helps reduce the strain on the colon while still providing some hydration and minimal nutrients.
- Bone Broth with Antimicrobial Herbs: Incorporating bone broth into your diet during a flare is beneficial. Bone broth is easy to digest, nourishing, and provides essential nutrients. Adding antimicrobial herbs like garlic, ginger, and thyme helps combat infection and inflammation.
- Gradual Reintroduction of Insoluble Fiber: Once symptoms start to improve, gradually reintroduce insoluble fiber into your diet. Start with small amounts and increase slowly to avoid overwhelming the digestive system.
- Long-Term Management: Emphasize a High-Fiber Diet
- High Fiber Intake: A diet rich in fiber is crucial for long-term management of diverticulosis. Fiber adds bulk to the stool, making it easier to pass and reducing pressure on the colon walls. Women should aim for at least 25 grams of fiber per day, while men should aim for 38 grams.
- Sources of Fiber: Incorporate a variety of fiber-rich foods into your diet, including fruits, vegetables, whole grains, legumes, nuts, and seeds. Foods like oatmeal, beans, broccoli, and pears are excellent choices.
- Balance of Soluble and Insoluble Fiber: While both types of fiber are important, soluble fiber (found in foods like oats, apples, and carrots) helps soften stool and is easier on the digestive system, especially after a flare.
- Incorporate Anti-Inflammatory Foods
- Anti-Inflammatory Diet: Long-term dietary management should include foods that reduce inflammation, which helps prevent future flares of diverticulitis. Focus on foods rich in omega-3 fatty acids (like salmon, flaxseeds, and walnuts), antioxidants (found in berries, leafy greens, and nuts), and other anti-inflammatory nutrients.
- Limit Pro-Inflammatory Foods: Avoid or limit foods that promote inflammation, such as processed foods, red meat, and foods high in refined sugars and unhealthy fats.
- Ensure Adequate Hydration
- Stay Hydrated: Adequate hydration is essential for a high-fiber diet to be effective. Moreover, fiber absorbs water, which helps soften stool and makes it easier to pass. Aim to drink at least 8-10 glasses of water daily, but adjust based on your fiber intake and physical activity level.
- Hydrating Foods: In addition to drinking water, include hydrating foods like cucumbers, watermelon, and soups in your diet to help meet your fluid needs.
- Gradual Dietary Adjustments
- Introduce Changes Slowly: If you’re not used to a high-fiber diet, make changes gradually. Rapidly increasing fiber intake leads to bloating, gas, and discomfort. Start with small additions and gradually increase over weeks or months.
- Monitor Your Body’s Response: Pay attention to how your body responds to different foods and adjust your diet accordingly. Everyone’s digestive system is different, so it’s important to find what works best for you.
- Consistency is Key
- Maintain a Consistent Diet: To effectively manage diverticulosis and prevent diverticulitis flares, consistency in your diet is crucial. Stick to a high-fiber, anti-inflammatory diet, and avoid drastic changes that could disrupt your digestive system.
- Regular Meal Times: Eating at regular intervals can help regulate bowel movements and prevent strain on the colon.
Supplements and Probiotics Treatment Approaches for Diverticulosis and Diverticulitis
Probiotics: Probiotics, particularly strains like Lactobacillus casei and Escherichia coli Nissle 1917, are beneficial for maintaining gut health and prolonging remission in diverticular disease. These strains help balance the gut microbiome, reducing inflammation and the risk of flare-ups.
L-Glutamine: This amino acid supports gut lining integrity, helping to repair damage caused by inflammation or infection. It can enhance the healing process, particularly during recovery from diverticulitis flares.
Mucilaginous Herbs: Herbs like slippery elm and marshmallow root create a soothing, protective coating along the digestive tract. Moreover, this reduces irritation and provides relief from symptoms like abdominal discomfort and bloating.
Butyrate: Butyrate, a short-chain fatty acid is crucial for colon health. Furthermore, it helps maintain the integrity of the colon lining and has anti-inflammatory properties, making it beneficial for those with diverticular disease.
Fiber Supplements: For those struggling to get enough fiber from diet alone, supplements like psyllium husk help ensure a regular and soft stool, reducing the strain on the colon and preventing the formation of new diverticula.
Additional Considerations for Diverticulosis and Diverticulitis Management
Magnesium Insufficiency: Low magnesium levels contribute to constipation, a common issue in diverticular disease. Supplementing with magnesium glycinate or citrate helps ease bowel movements. Glycinate is often better for those with looser stools, while citrate is more effective for relieving constipation.
Chewing and Eating Hygiene: Proper chewing is crucial for digestive health, especially for those with diverticular disease. Moreover, chewing food thoroughly reduces the strain on the digestive system, helping to prevent the formation of new diverticula and easing discomfort during digestion.
Avoiding Certain Foods Temporarily: During active diverticulitis, it’s advisable to avoid hard-to-digest foods like corn, whole seeds, and certain grains. These irritate the gut or get trapped in diverticula, potentially worsening inflammation. Gradual reintroduction of these foods should occur once the acute phase subsides
Conclusion
Managing diverticulosis and diverticulitis requires a multifaceted approach that includes dietary modifications, supplementation, and lifestyle changes. A high-fiber diet, proper hydration, and the use of probiotics and supplements like magnesium and butyrate help maintain digestive health and prevent flare-ups. Additionally, paying attention to eating habits, such as thorough chewing, and temporarily avoiding certain foods during active diverticulitis, reduces the risk of complications. By adopting these strategies, individuals with diverticular disease improve their quality of life and better manage their condition over the long term.