Functional Medicine Approach For Ulcerative Colitis
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum, causing inflammation and ulcers in the digestive tract. This condition significantly impacts a patient’s quality of life due to its chronic nature and the severity of symptoms. A functional medicine approach, which focuses on identifying and addressing the root causes of disease, offers an integrative and holistic treatment strategy for UC. This blog will explore UC’s symptoms, causes, risk factors, conventional treatments, and functional medicine interventions, including dietary changes, nutritional supplements, and probiotics.
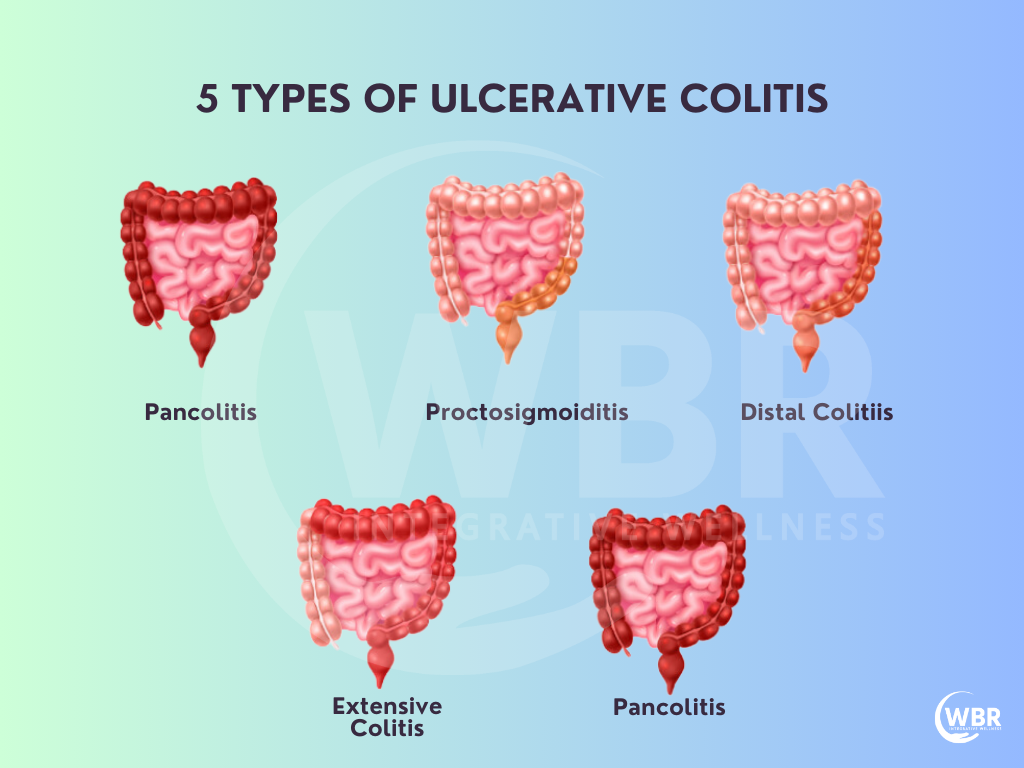
What is Ulcerative Colitis?
Ulcerative colitis is an autoimmune condition where the immune system mistakenly attacks the lining of the colon, leading to inflammation and ulceration. Unlike Crohn’s disease, which is capable of affecting any part of the gastrointestinal tract, UC is confined to the colon and rectum. The exact cause of UC is unknown, but it is believed to result from a combination of genetic, environmental, and immune factors.
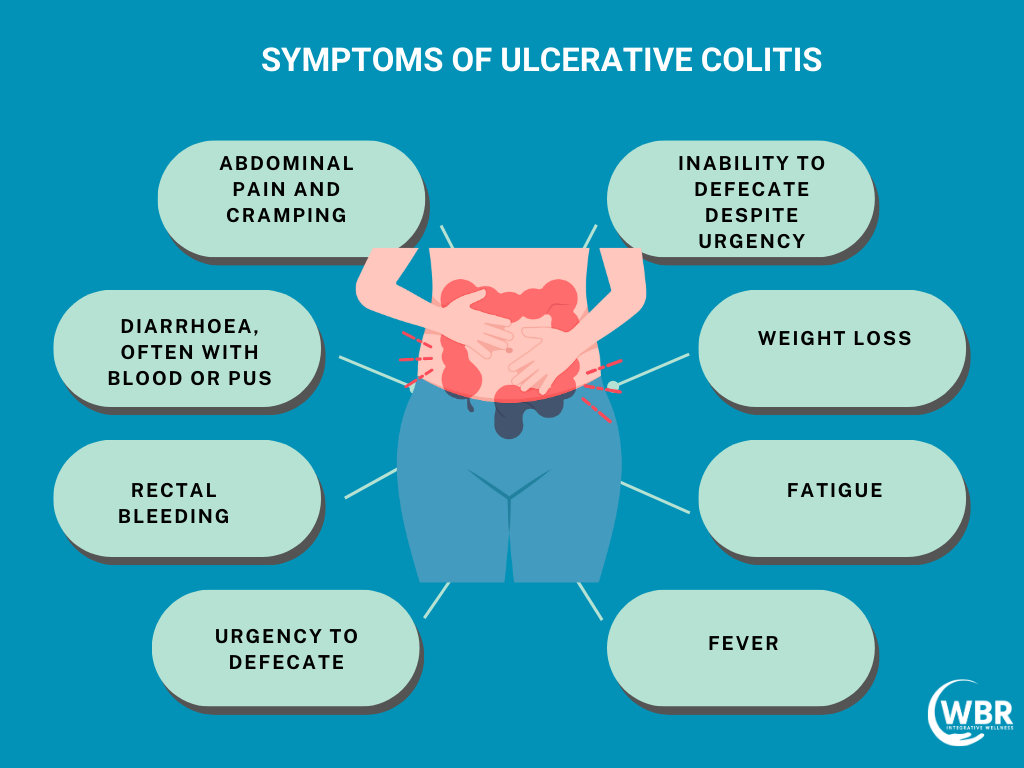
Symptoms of Ulcerative Colitis
Ulcerative Colitis (UC) manifests through a range of distressing symptoms. Understanding these signs is pivotal for early diagnosis and effective management.
Persistent Diarrhea: Frequent, urgent bowel movements often contain blood or pus, which can lead to dehydration and discomfort.
Abdominal Pain: Cramping and persistent discomfort, typically focused in the lower left side of the abdomen, arising during flare-ups.
Rectal Bleeding: Blood in stool or during bowel movements, a hallmark symptom of UC.
Weight Loss: Unexplained weight loss due to malabsorption of nutrients or reduced appetite during active disease phases.
Fatigue: Ongoing tiredness, which can be severe and debilitating during UC flare-ups.
Fever: Low-grade fever may accompany inflammation during disease exacerbations.
Loss of Appetite: A diminished desire to eat, leading to nutritional concerns.
Joint Pain: Some individuals experience joint pain or swelling, although this is less common.
Skin and Eye Problems: Inflammatory skin conditions, eye inflammation (uveitis), and mouth sores can occasionally co-occur with UC, reflecting its systemic impact.
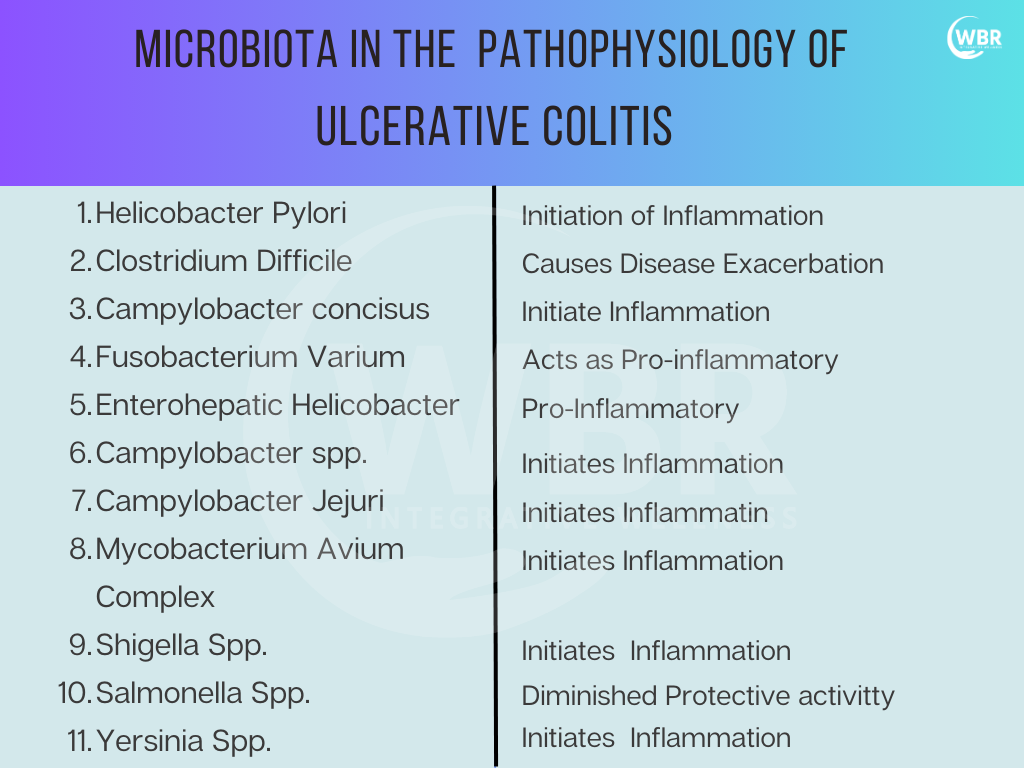
Causes of Ulcerative Colitis
While the exact cause remains unclear, genetic and environmental factors are thought to play a role. Let us look at some of the most common and specific causes that lead to Ulcerative Colitis
Enterohepatic Helicobacter Species: Emerging research suggests a possible link between certain Helicobacter species residing in the digestive tract and UC development. These bacteria trigger abnormal immune responses leading to chronic inflammation.
Infections: Prior infections or dysregulation of the immune system in response to pathogens play a role in UC development. Researchers are investigating the relationship between infections and subsequent inflammatory bowel diseases.
Certain Medications: Some medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), exacerbate UC symptoms or trigger flare-ups in susceptible individuals.
Family History/Genetics: A significant factor in UC risk is genetic predisposition. Individuals with family members suffering from Ulcerative Colitis are at a higher risk of developing the condition themselves.
Tobacco Use: Smoking is linked to an increased risk of this condition, and it also exacerbates the severity of the disease in those already affected.
Diet: Diet plays a role in Ulcerative Colitis management, but its precise influence on disease onset remains under investigation. Some dietary factors exacerbate symptoms or contribute to inflammation.
Fecal Sulfur Metabolome: The composition of sulfur metabolites in the gut has some implications for UC development. Understanding the role of these metabolites is an evolving area of study in the context of inflammatory bowel diseases.
Risk Factors of Ulcerative Colitis
While the exact cause of Ulcerative Colitis remains unclear, several factors are believed to contribute to its development and exacerbation.
- Dietary Factors: Diet plays a significant role in managing Ulcerative Colitis, with several considerations for patients:
- Malnutrition Risk: Chronic diarrhoea, inflammation, and medication use lead to malnutrition. Thus, it’s essential to assess and supplement protein, calories, and micronutrients.
- Fluid Intake: Maintaining liberal fluid intake is crucial to prevent dehydration.
- Symptom Aggravation: Certain foods worsen symptoms, including cruciferous vegetables, raw or spicy foods, high-fibre foods, nuts, seeds, caffeine, alcohol, and carbonated beverages. Hence, small, frequent meals are recommended to ease digestion.
Food Allergy
Food allergies play a significant role in the pathogenesis of Ulcerative Colitis. Moreover, increased histamine and IgE levels in the colonic mucosa suggest that food allergens might trigger or exacerbate symptoms. Common allergens include cow’s milk, wheat, eggs, corn, and citrus fruits. Furthermore, avoidance of these foods often leads to remission or improvement in symptoms.
Lactose Intolerance
Lactose intolerance is prevalent among Ulcerative Colitis patients, with rates ranging from 8% to 59%. While lactose intolerance itself is not a cause, it often exacerbates symptoms, making it important for patients to manage their lactose intake.
Other Sensitivities
- Salicylate Sensitivity: This is one common type of sensitivity found in ulcerative colitis. Hence, some patients improve on a low-salicylate diet.
- Carrageenan: Found in processed foods, carrageenan often causes colonic lesions in animals and could be unsafe for Ulcerative Colitis patients. Thus, a carrageenan restrictive diet is often recommended for patients of UC.
Nutritional Supplements
Nutritional supplements play a crucial role in managing Ulcerative Colitis by addressing deficiencies and supporting overall health.
Fish Oil
Fish oil has anti-inflammatory properties, and most studies show clinical improvement and decreased medication requirements in Ulcerative Colitis patients. Typically, high doses (6 g/day) are used, but smaller doses might also be beneficial.
Folic Acid
Folic acid deficiency is common due to sulfasalazine use and the disease itself. Moreover, a chronic deficiency increases the risk of colon cancer, and supplementation might decrease its incidence.
Zinc
Ulcerative Colitis patients often have low serum zinc levels, although results are mixed. Moreover, zinc supplementation might have anti-inflammatory benefits.
Magnesium
Ulcerative Colitis patients are at risk of magnesium deficiency due to diarrhoea and postoperative periods. Symptoms of deficiency include fatigue, muscle spasms, and chronic constipation.
Vitamin B6
Low levels of vitamin B6 are common in Ulcerative Colitis patients and may contribute to thromboembolic disease. Moreover, intravenous administration has shown marked improvement in muscle weakness.
Vitamin A
Low levels of vitamin A are found in the patients, and a proper dose often leads to improvements in symptoms and risk factors associated with the disease.
Iron
Iron deficiency is common in UC patients and often leads to anaemia. Moreover, intravenous iron is more effective and better tolerated than oral iron.
Vitamin K
A significant portion of patients suffering from this disease have vitamin K deficiency. Moreover, Vitamin K supplementation might help prevent osteoporosis.
Vitamin D
Low levels of vitamin D are common in patients who suffer from this disease. Furthermore, supplementation should be considered with a proper dosage to see the results.
Vitamin B12, B9, B1, B2, B5 and B6
Vitamin B12 and others can help for energy, weakness, mood changes, and for symptoms like tingling in the fingers and toes
Propionyl-L-Carnitine (Colon Release)
Fatty acid oxidation is impaired in patients suffering from this disease, and supplementation with propionyl-L-carnitine improves clinical outcomes.
Phosphatidylcholine (Delayed Release)
Phosphatidylcholine protects the mucus layer and is beneficial for glucocorticoid-dependent and non-glucocorticoid-treated UC patients.
Vitamin E
A vitamin E metabolite specially mixed tocopherols can help to reduce inflammation and protecting cell membranes. This can be helpful along with phytosome.
Herbs and Plants to Manage UC
Many herbs and plant extracts have shown promise in mitigating symptoms of Ulcerative Colitis and promoting gut health.
Aloe Vera Gel: Aloe vera’s anti-inflammatory properties can soothe UC-related intestinal irritation when consumed in controlled amounts.
Butyrate: This short-chain fatty acid, often lacking in UC patients, supports colon health and may reduce inflammation. Butyrate enema can also be planned if possible.
Tormentil Extracts: Rich in tannins, tormentil extracts possess astringent and anti-inflammatory qualities, potentially aiding UC symptom relief.
Wheat Grass Juice: The chlorophyll-rich wheatgrass juice may assist in meeting multi nutrient needs.
Phytosome Curcumin: Curcumin with phospolipids has strong anti-inflammatory properties and can help to reduce pain and inflammation. Effective dose can be at 6-8 grams per day split into 2-3 times and to be started slow.
Triticum Aestivum (Poaceae): A type of wheatgrass, it may help in reducing inflammation and oxidative stress.
Acanthaceae: This herb has shown anti-inflammatory and immune-modulating potential in UC.
Boswellia Serrata: Boswellia extracts contain compounds that may alleviate inflammation and improve UC symptoms.
Extract of Myrrh: Myrrh extract exhibits anti-inflammatory properties that could be beneficial for UC symptom management.
Dry Extract of Chamomile Flowers: Chamomile’s soothing and anti-inflammatory qualities may provide relief from UC-related discomfort.
Metagenics UltraInflamX Plus 360: Take daily (2 scoops serving) to provide nutritional, amino acids and antioxidant needs as GUT nutrient absorption is not optimal twice daily for 2-3 months.
GI Revive or Repair: Take daily (1 scoops serving) to soothe and heal the gut mucosal lining for a period of 3-4 months, this to be kept away from food, best is empty stomach in morning. GI Revive is formulated with specific amino acids, botanical extracts, and minerals to offer comprehensive support for gastrointestinal (GI) health and function. It is combination of L-glutamine, an amino acid that provides structural and metabolic support for intestinal cells, zinc L-carnosine which provides support for the health of the intestinal lining, N-acetyl-D-glucosamine supports a normal inflammatory response in the GI tract. It also contains a botanical blend of deglycyrrhizinated licorice (DGL) extract, aloe vera, marshmallow, okra extract, and cat’s claw that provides support for healthy intestinal function by coating and soothing the intestinal lining.
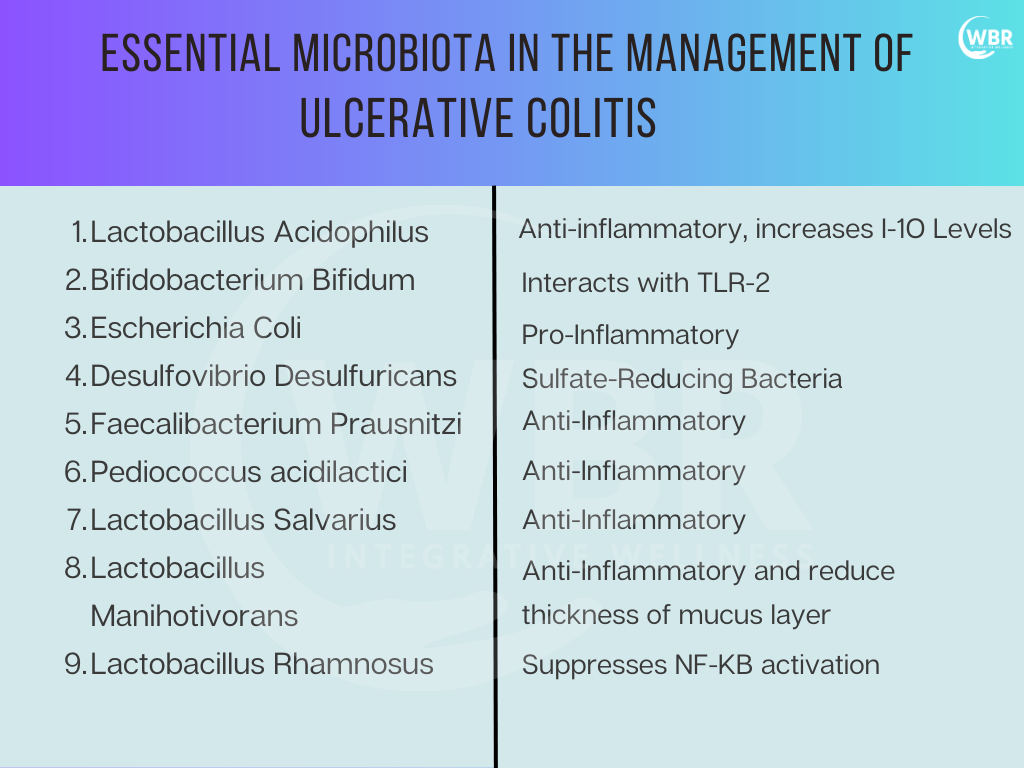
Probiotics for Management of Ulcerative Colitis
Probiotics are garnering attention as potential allies in the management of Ulcerative Colitis (UC). Among these beneficial bacteria strains, Lactobacillus Plantarum, Bifidobacterium Infantis, Lactobacillus Rhamnosus, and VSL#3 show promise in supporting UC patients.
Lactobacillus Plantarum (299v): Renowned for its anti-inflammatory properties, Lactobacillus Plantarum may help modulate the gut microbiome, fostering balance and potentially alleviating UC symptoms.
Bifidobacterium Infantis: This probiotic strain promotes gut health by enhancing beneficial bacterial populations while reducing harmful microbes. It shows potential in reducing inflammation commonly associated with UC, offering relief to patients.
Lactobacillus Rhamnosus: Known for its immune-boosting qualities, Lactobacillus Rhamnosus enhances immune function and maintain a balanced gut environment. This could contribute to managing UC more effectively.
Visbiome: A potent probiotic cocktail, Visbiome, is effective in UC management. By promoting gut microbial diversity and reducing inflammation, it offers a comprehensive approach to symptom relief and improved well-being for UC patients.
Visbiome, Lactobacillus plantarum 299V, Bifidobacterium longum 35624, E-coli Nissle1917, L.Reuteri (DSM 17938, ATCC 6475) , L.Gasseri ( BNR17) Include these probiotic strains to support gut health and improve the body’s response to adrenaline surges.
Note: Supplement recommendations should be personalised based on the individual’s current condition, whether in a flare or remission, and their unique comorbidities and nutritional needs.
Tips for Managing Ulcerative Colitis with a Functional Medicine Approach
- Dietary Modifications: Avoid trigger foods, maintain balanced nutrition, and consider an elimination diet to identify food sensitivities.
- Nutritional Supplements: Address specific deficiencies with targeted supplementation, such as fish oil, folic acid, zinc, magnesium, vitamins B6, A, K, D, iron, and others.
- Probiotics: Incorporate probiotics like VSL#3 and Lactobacillus rhamnosus GG to promote gut health and reduce inflammation.
- Hydration: Moreover, ensure adequate fluid intake to prevent dehydration.
- Stress Management: Practice stress-reducing techniques like meditation, yoga, and mindfulness, as stress exacerbates symptoms.
- Regular Monitoring: Furthermore, you need regular check-ups with a healthcare provider to monitor disease progression and adjust treatment as needed.
- Holistic Approach: Combine dietary changes, supplementation, probiotics, and stress management for a comprehensive approach to managing Ulcerative Colitis.
Lifestyle Support for Ulcerative Colitis
- Smaller, Intentional Meals: Eat five or six small meals a day to avoid overloading the digestive tract and reduce stress while eating.
- Stress Reduction: Manage stress to prevent IBD flare-ups by balancing stressful areas of life.
- Rest and Sleep: Prioritize sleep and rest to lower stress.
- Support Systems: Encourage participation in support groups or connections with others who understand IBD.
- Journaling: Track daily habits, foods, emotions, and symptoms to identify patterns and triggers.
- Mind-Body Therapy: Incorporate daily meditation and stress-reduction practices to help manage UC symptoms.
- Acupuncture: Schedule regular acupuncture sessions to reduce inflammation and improve gut health.
- Moxibustion: Moxibustion is a traditional Chinese medicine therapy that involves burning dried mugwort (moxa) near or on specific points of the body. Use moxibustion therapy to support immune function and alleviate gastrointestinal discomfort.
The role of diet in the prevention and treatment of Inflammatory Bowel Diseases
Diet plays a pivotal role in the prevention and management of Inflammatory Bowel Diseases (IBD). Understanding its impact on gut microbiota, immunity, and the disease itself is crucial for comprehensive care.
The Role of Diet in Prevention and Treatment: Diet profoundly influences IBD, with certain foods triggering or mitigating symptoms. Tailoring dietary choices significantly impacts disease management.
Gut Microbiota and IBD: A balanced gut microbiome is essential for immune regulation. Dysbiosis, or microbial imbalance, is linked to IBD development and severity.
Immunity and IBD: Dysregulated immune responses contribute to IBD. Diet can modulate immunity, either exacerbating inflammation or promoting healing.
Diet and IBD: Specific dietary interventions, like low-residue or anti-inflammatory diets, can alleviate symptoms and improve the quality of life for individuals with IBD.
Role of Enteral Nutrition in Remission and Symptom Control: Enteral nutrition involves delivering nutrients in a liquid form that is easily absorbed by the gut. This approach is especially effective in inducing remission in patients with Irritable Bowel Diseases like Ulcerative Colitis, notably in children. It minimizes the need for corticosteroids and other medications by directly providing essential nutrients, allowing the gut to rest and heal.

Dietary Support Guidelines for Ulcerative Colitis
General Approach: Follow healthcare providers’ guidelines while considering individual needs.
- Dairy-free
- Lower fat
- Paleo
- Ayurvedic
- Mediterranean
- Elimination diet (to identify trigger foods)
Pantry Staples to include in your diet
- Easier-to-digest fruits (bananas, cooked fruits, cantaloupe)
- Lean proteins (fish, white meat poultry, eggs)
- Fully cooked, seedless, skinless vegetables
- Stocks and broths
- “Clean” meats (organic, no added hormones or antibiotics)
- Soothing herbs (ginger, lavender, chamomile)
Foods to Avoid
- Alcohol and caffeine
- Carbonated beverages
- Gluten and grains (varies individually)
- Conventional dairy products
- Processed foods
- Fatty, greasy foods
- Artificial sweeteners and processed sugar
- “Hot” spices (pepper, chiles, cayenne, cumin)
- During flare-ups: nuts, seeds, and corn
Diets for Managing Ulcerative Colitis
- Specific Carbohydrate Diet (SCD): Focuses on eliminating complex carbohydrates and sugars to reduce inflammation and support gut healing. Emphasises natural, nutrient-dense foods like meats, fruits, vegetables, and nuts.
- Autoimmune Protocol (AIP): Eliminates potential inflammatory foods such as grains, dairy, legumes, and nightshades to help reduce autoimmune responses and promote gut healing. Gradually reintroduces foods to identify triggers.
- Paleo Diet: Emphasizes whole, unprocessed foods like lean meats, fish, fruits, vegetables, nuts, and seeds, while excluding grains, legumes, and dairy. Aims to reduce inflammation and support overall health.
- Mediterranean Diet: Rich in proteins, healthy fats (especially EVOO), and high-fibre foods like lentils, legumes, and vegetables. Encourages the consumption of anti-inflammatory foods high in omega-3s and phytochemicals to support gut health and reduce inflammation.
Additional Dietary Considerations for Ulcerative Colitis
- To address malnutrition, assess nutritional status and supplement protein, calories, and micronutrients as needed.
- Identify specific foods that worsen symptoms and avoid them to manage Ulcerative Colitis better.
- Evaluate for food allergies, as they may trigger or exacerbate symptoms; common allergens include cow’s milk, wheat, eggs, and corn.
- Some patients may need to avoid lactose due to intolerance.
- Although rare, salicylate sensitivity can cause symptoms in some patients and should be considered.
- Avoid processed foods containing carrageenan, as it may cause ulcerative lesions.
- Wheat grass juice may improve disease activity in patients with ulcerative colitis.
Conclusion
A functional medicine approach to managing ulcerative colitis emphasizes addressing the root causes of the disease and supporting overall health through dietary modifications, nutritional supplements, and probiotics. By focusing on individual needs and promoting a holistic treatment strategy, patients with UC can achieve better symptom management, maintain remission, and improve their quality of life.