Probiotic Diet Therapy for Rheumatoid Arthritis
RA patients are often required to undergo long-term therapy. Though primarily efficacious, the treatment options of pharmaceutical drugs can yield unpleasant side effects. In relation to Rheumatoid Arthritis and other inflammatory disease, the patients suffer from an overproduction of pro-inflammatory cytokines and insufficient production of anti-inflammatory cytokines. Here in this blog we will share the top specific probiotic strains which are effective in decreasing RA activity. The best part is those specific strains can be fermented and consumed orally as part of diet.
Rheumatoid Arthritis is a common inflammatory disorder that affects the joints in the hands and feet. If you’re someone suffering from Rheumatoid Arthritis, you ought to be aware that it is tough on the body. Not only does it cause pain, but RA also makes it challenging to move around and perform daily activities. If you’re looking for ways to help manage RA, you might want to look into the probiotic approach. This treatment involves consuming high-quality probiotics to improve gut health and heal the body from the inside out. But before diving into the cure, let us look at the causes behind Rheumatoid Arthritis.
What causes Rheumatoid Arthritis?
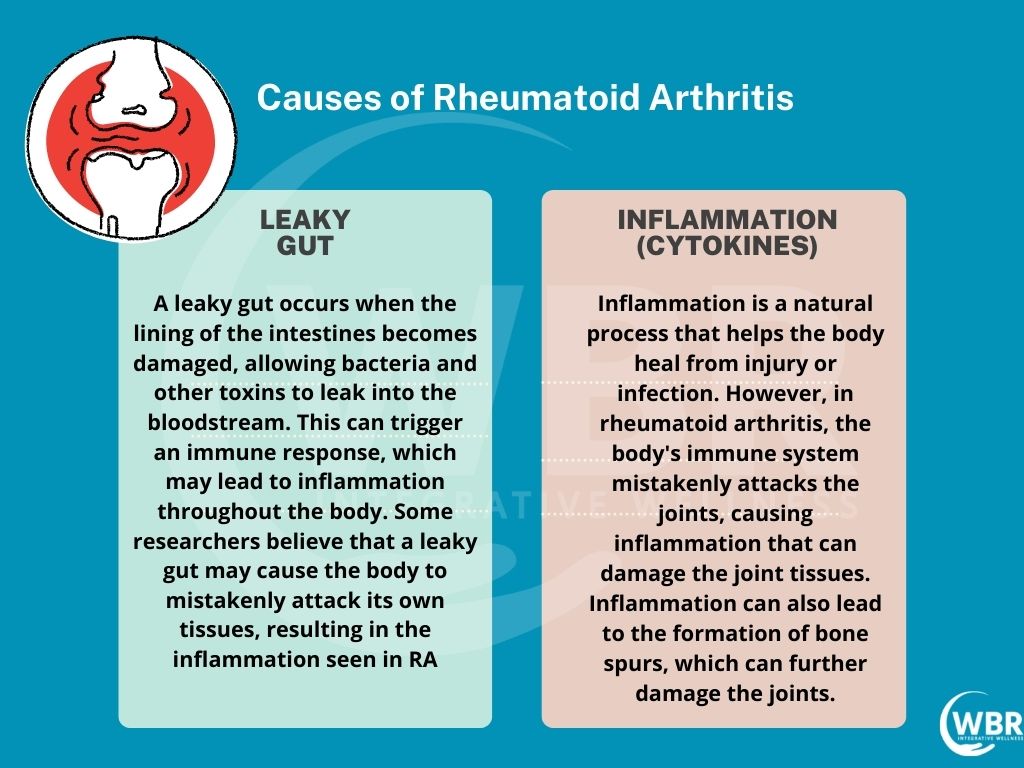
Rheumatoid Arthritis is an auto-immune disease which makes the human immune system attack healthy body tissues. The immune system fights foreign elements like viruses and bacteria in the body. But with a condition like Rheumatoid Arthritis, the immune system mistakes the necessary body cells for foreign components. It thus starts attacking the body cells with the release of inflammatory chemicals. Cytokines are one such inflammatory chemical that leads to the development of Rheumatoid Arthritis. There are two primary causes that lead to Rheumatoid Arthritis:
- Leaky Gut
- Inflammation (Cytokines)
What is Leaky Gut?
Leaky gut is a condition in which the lining of the intestines becomes damaged, allowing harmful substances to “leak” through into the bloodstream. These substances can trigger inflammation throughout the body, including in the joints, which can lead to rheumatoid arthritis.
There are a number of factors that can contribute to leaky gut, including a diet high in sugar and processed foods, chronic stress, and certain medications. Fortunately, there are also ways to heal leaky gut, which can in turn help to reduce the inflammation and pain associated with rheumatoid arthritis.
What are Cytokines?
Cytokines are a class of signaling molecules that play a crucial role in the immune system. They form a family of four lymphoid cells; interleukins(ILs), Tumor Necrosis Factors(TNFs), interferons(IFNs) and colony-stimulating factors(CSFs). Cytokines get produced in response to the immunological challenges from various sources like:
- Nutritional Deficiency
- Stress
- Physical Injury
- Infection
- Genotype
- Toxic Influences
Various cells produce Cytokines that include immune cells. They also help regulate the activity of the immune system. There are two types of Cytokines: pro-inflammatory cytokines and anti-inflammatory cytokines. Pro-inflammatory cytokines help to promote the inflammatory response, while anti-inflammatory cytokines help to reduce inflammation.
A large volume of Cytokines remains active in the joints of the patients who suffer from Rheumatoid Arthritis. Cytokines play a rudimentary role in causing the inflammation associated with Rheumatoid Arthritis. But recent study displays that the
Gut Microbiome and Rheumatoid Arthritis
There is growing evidence that the gut microbiome may play a role in the development of rheumatoid arthritis (RA). RA is a chronic inflammatory disease that affects the joints, and it is thought that gut dysbiosis (an imbalance in the gut microbiome) may contribute to the inflammation seen in RA. Studies have shown that patients with RA have a different gut microbiome than healthy individuals, and that gut dysbiosis may precede the onset of RA symptoms. Additionally, probiotic and prebiotic interventions (which can help to restore a healthy gut microbiome) have been shown to improve RA symptoms. Thus, the gut microbiome may be a potential target for the treatment of RA.
How do Probiotics help in Healing Rheumatoid Arthritis?
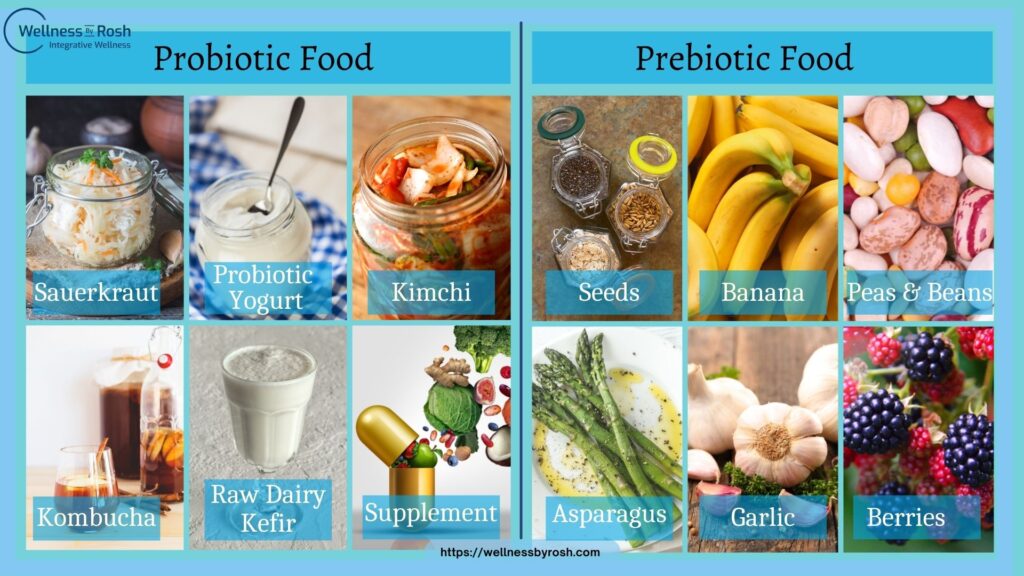
The human digestive system is replete with a good balance of bacteria. These bacteria, also known as gut microbiota, help to digest, thereby maintaining good health. Probiotics form a group of living bacteria present in our food and supplements.
People suffering from Rheumatoid Arthritis often experience inflammation in the intestine. The burning sensation in the intestine usually leads to gut permeability. The gut permeability is often responsible for leaking harmful bacteria from the digestive system to other body parts. Probiotics play a vital role in reducing the inflammation caused due to Rheumatoid Arthritis. Probiotics thus help restore the balance of digestive microbiota.
The gut bacteria grow with prebiotic fibres. The prebiotic fibres allow the gut bacteria to create healthy byproducts such as SCFA. Short chain fatty acids (SCFAs) are a type of fatty acid that are produced when the gut bacteria breaks down dietary fiber. SCFAs have been shown to have anti-inflammatory effects and have been suggested as a potential therapy for inflammatory diseases such as rheumatoid arthritis (RA).
Benefits of Probiotics Approach to Rheumatoid Arthritis
The summary of top benefits for specific probiotic approach for people suffering with R.A are
- Limitation of inflammatory cytokine production.
- Reduce the production of several pro-inflammatory molecules: IL-1β, IL-2, IL-6, IL-12, IL-17, IFN-γ andTNF-α.
- Significant increase in the most potent anti-inflammatory interleukin IL-10 levels.
- Reduce inflammatory markers like CRP, ESR, Rheumatoid Factor.
- Protection against pathogens and their toxins by regeneration of mucosal cells.
- Prevention of stress-induced alterations to overall intestinal microbiota.
- Limitation of carbohydrate malabsorption.
- Increases collagen and bone density, prevent osteoporosis.
- Regulate hormone oxytocin and healthy immune responses .
- Improvement of nutritional status.
- Minimising the side effects of pharmaceuticals drugs if any.
- Accelerating the treatment of some intestinal infections.
- Assisting in the reduction of gas and bloating.
- Preventing or minimising the severity of colds and flu.
- Play complimentary role in eradication of H.Pylori, fungal overgrowth (IMO, SIFO).
- Increases the production of glutathione – an important antioxidant.
- Improves bowel regularity. Provides relief of both diarrhea, constipation, IBS.
- Increases gastrointestinal mannitol production through the consumption of glucose and fructose. Mannitol prevents the aggregation of harmful proteins.
- It mitigate the symptoms of maldigestion induced by genetic or acquired enzyme deficiencies.
- Increases gastrointestinal mannitol production through the consumption of glucose and fructose. Mannitol prevents the aggregation of harmful proteins.
- Ability to degrade glyphosate to carbon, phosphate and water, and removes heavy metals such as aluminium.

Different Probiotics Approaches
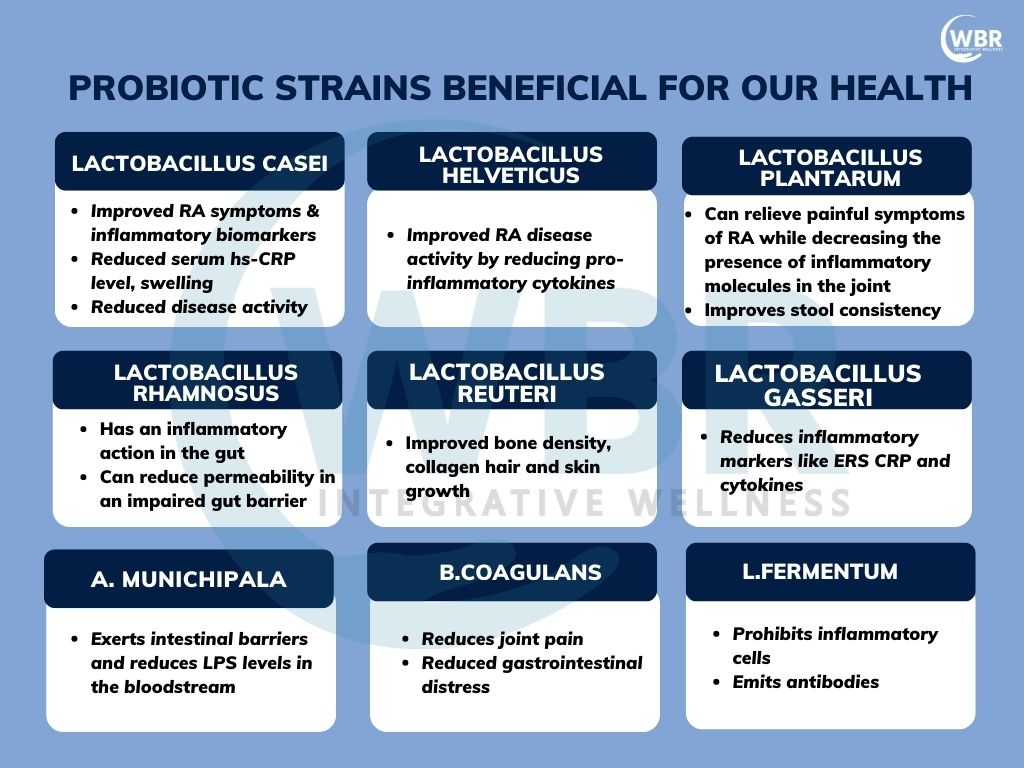
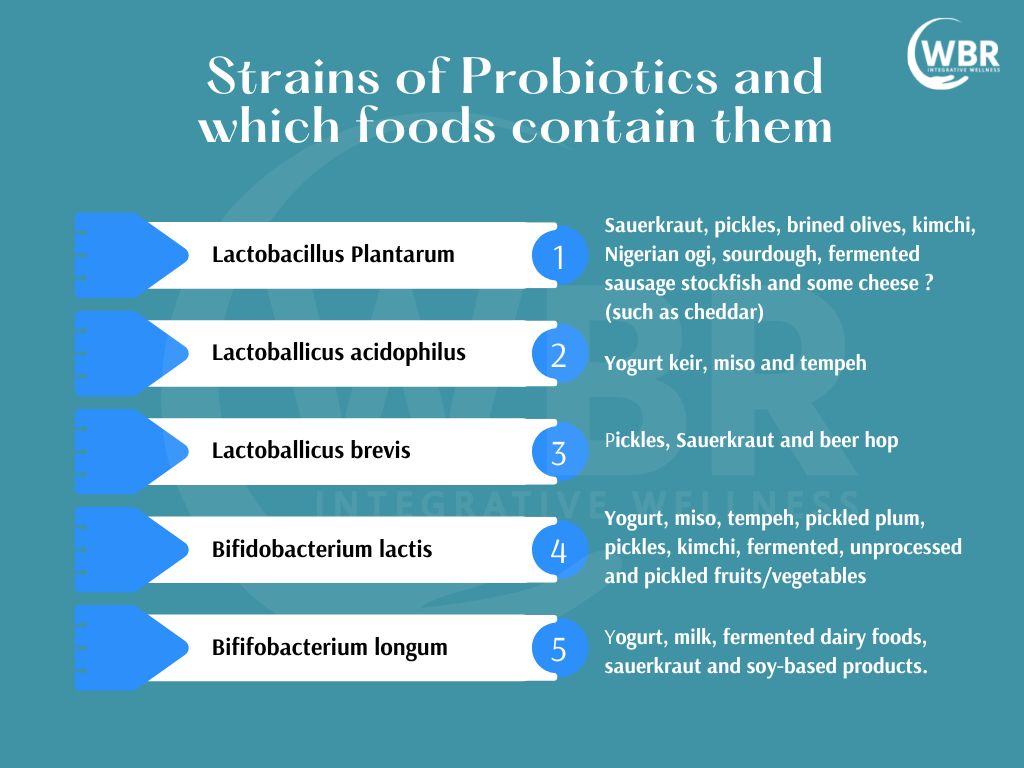
Probiotics are one of several available nutritional supplements that may provide adjuvant therapy for RA. It is found to have a positive relationship between oral administration of certain probiotic strains and decreased RA disease activity. These studies differ by probiotic strain and dose. They highlight the most favourable observations for each strain are as follows.
-
Lactobacillus casei:
The supplementation of Lactobacillus Casei (L. Casei) improved RA symptoms and inflammatory biomarker, had reduced serum hs-CRP levels, less swollen and tender joints, and reduced disease activity. There was also a significant improvement in the anti-inflammatory IL-10 levels.. L. casei inhibited the production of several pro-inflammatory molecules: IL-1β, IL-2, IL-6, IL-12, IL-17, IFN-γ andTNF-α.
-
Lactobacillus helveticus:
L. helveticus effectively reduced CII-reactive immunoglobulin antibodies, improved disease activity by reducing proinflammatory cytokines TNF-α, IFN-γ, and IL-17A and enhancing IL-10 expression. This can be given/fermented along with Bifidobacterium longum (B. longum), and Lactobacillus johnsonii (L. johnsonii).
-
Lactobacillus plantarum:
L. plantarum displayed improvements in all parameters ( (ESR), C-reactive protein (CRP), rheumatoid factor (RF), and serum TNF-alpha). L. plantarum can relieve painful symptoms of arthritis while decreasing the presence of inflammatory molecules in the joints. It also improves joint health and mobility.
-
Lactobacillus rhamnosus (ATCC 53103):
was associated with a reduced number of swollen and tender joints, bacteriocin production, inflammation reduction, food allergies/hypersensitivity reduction, increased intestinal mucus lining.
-
Bacillus coagulans (GBI-30, 6086):
This microbe produces proteins known as bacteriocins and lactic acid that lowers local pH levels. This process may eliminate some of the microbes that contribute to an inflammatory response in the host. B. coagulans also produces a butyric acid, a short-chain fatty acid, that aids in the healing process of cells in the small and large intestines. The B. coagulans decreases IL-1 beta and TNF-α proinflammatory cytokines.It may act in a similar way by lowering prostaglandin production to activate antiinflammatory cytokines. It helps in reduction of arthritis pain, CRP reduction and thus indicating a reduction in RA disease activity.
-
L.Gasseri ( BNR17):
This probiotic species produces a bacteriocin effective against select species of Enterobacteriaceae. reduced symptoms of “functional dyspepsia” (bothersome postprandial fullness, early satiety, epigastric pain, and epigastric burning, also suspicious for undiagnosed SIBO). This also helps in reducing ESR, CRP and other inflammatory cytokines.
-
Akkermansia muciniphila (WB-STR-0001):
This reduces LPS levels in the blood stream, increase intestinal mucus lining. Akkermansia populations are increased with prebiotic fiber and polyphenol intake (e.g., berries, peppers).
-
L.Fermentum (ME-3):
This strain prohibits inflammatory cells, emit antibodies, antibiotic stimulants, altering Th1/Th17 responses. This strain is able to produce nitric oxide (NO) The NO is able to induce among others the protection against inflammation. This protect the host from different diseases induced by pathogenic bacteria (Salmonella spp., Shigella spp. and urinary tract infections cause by E. coli), inflammation and oxidative stress. L.Fermentum helps in synthesising of tripeptide antioxidant- Glutathione.
-
Saccharomyces boulardii ( CNCM-I75):
This is a friendly yeast. Moreover, it is a key addition for spectrum of favourable health benefits including prebiotic effects, nutrient digestion and absorption, toxin degradation, pathogen reduction, healthy microbiome, support strong immune system, play complimentary role in eradication of H.Pylori, fungal overgrowth (IMO, SIFO), reduces the risk to develop diarrhoea and reduce antibiotics side effects.
-
L.Reuteri (ATCC PTA 6475 and DSM 17938):
The most powerful of all to boost oxytocin, support in deeper sleep, reduction in stress, increases collagen, muscle and bone density, reduce SIBO, constipation, digestive disorder, reduce inflammation, enhances immunity.
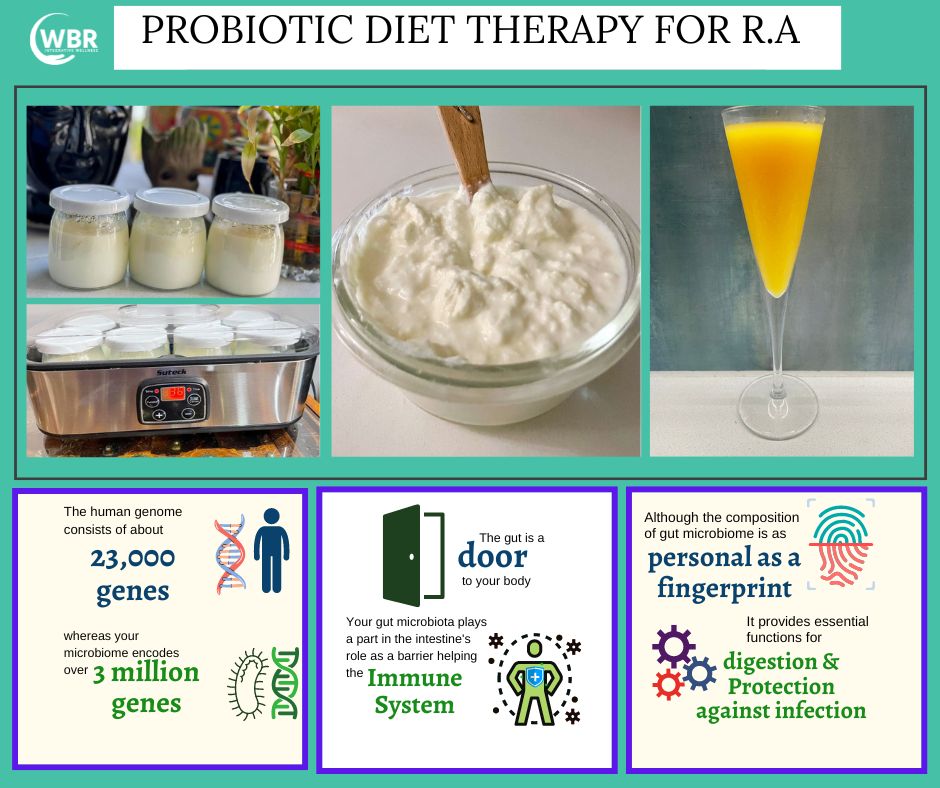
Daily Doses
It is recommended to co-ferment these strains at temperature of 104-106 F in order to have maximum benefit as high CFUs counts are needed to show immediate effect. Except Akkermansia which is anaerobic all other strains can be fermented in dairy or non dairy sources. Extended fermentation 24-48 hours needed to get the right quantity per cup.
1-2 cup mix with multiple probiotic yoghurts of different specific strains.
Regular intake of prebiotic fibre Inulin, FOS, Acacia Senegal, Pectin
Timing
There is no specific time. Keep 4 hours from any anti-microbial supplements such as iodine etc.
Conclusion
In relation to RA, probiotics are believed to affect the imbalance of cytokine production that is known to cause inflammation and pain in RA patients. Thus, it is essential that the commensal bacteria maintain local homeostasis with the host’s intestinal immune system. The gut normally provides protection against antigens from many microorganisms. The primary focus of probiotic diet therapy for RA is to heal the microbiome and restore a healthy immune system.It is an effective way to decrease the symptoms, reduce any side effects of existing conventional medications, and adverse effects of the condition.
References
https://www.ncbi.nlm.nih.gov/books/NBK441999/
https://www.sciencedirect.com/topics/medicine-and-dentistry/rheumatoid-arthritis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6223323/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2670518/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8539185/
https://academic.oup.com/jn/article/145/7/1446/4589930
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2826289/
https://www.sciencedirect.com/science/article/abs/pii/S1075996414001231?via%3Dihub